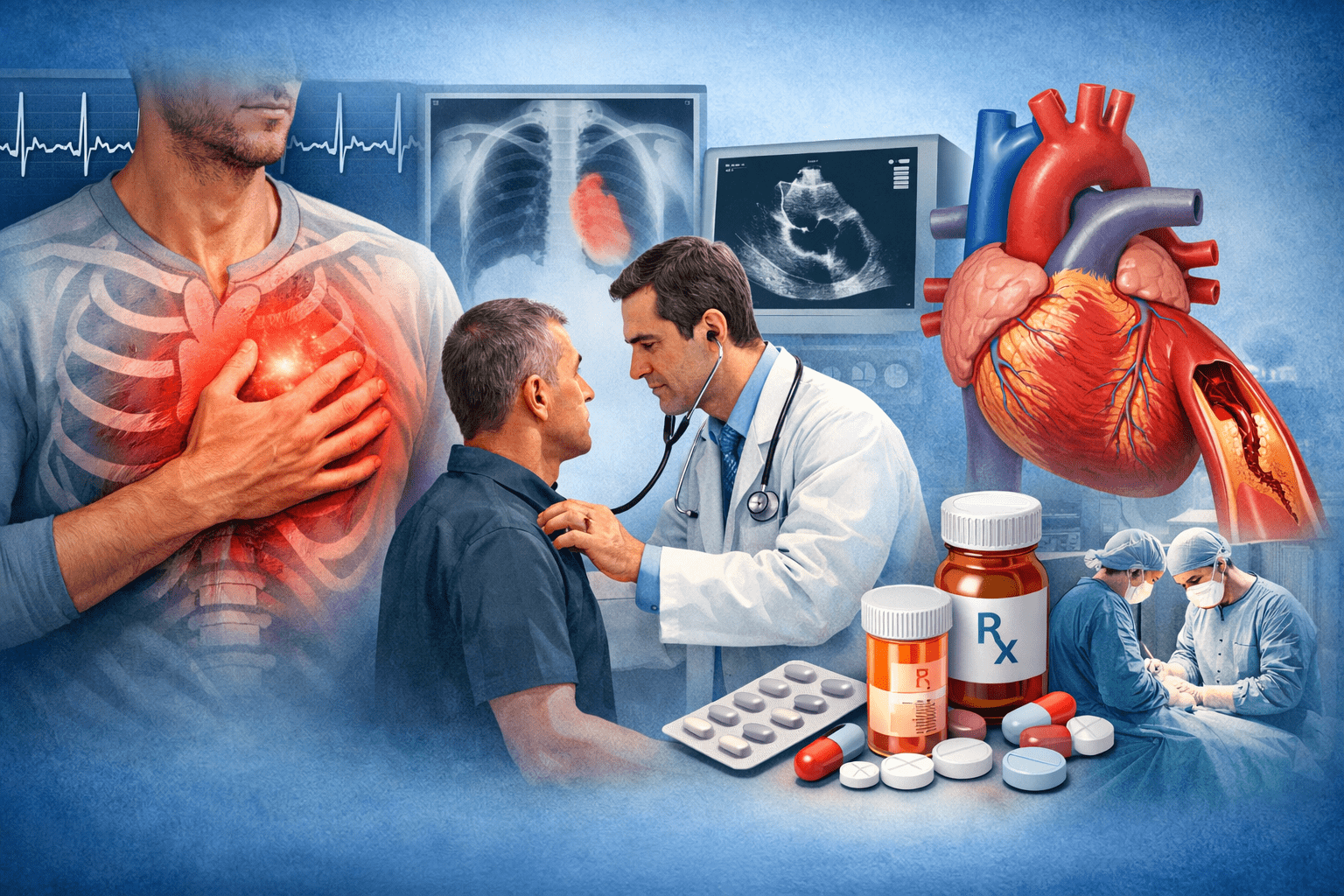
Chest pain is one of the most alarming symptoms a person can experience. For many, it immediately raises fear of a heart attack—and while that concern is sometimes valid, chest pain doesn’t always originate from the heart. Understanding the wide range of chest pain causes is essential, as the discomfort may stem from cardiac, digestive, muscular, or even stress-related conditions. Over the years, I’ve seen patients delay care out of uncertainty, and others rush to the emergency room for pain that had nothing to do with their heart at all.
Understanding chest pain—what causes it, how it’s evaluated, and when it requires urgent attention—can make a critical difference. From a cardiologist’s perspective, clarity saves lives.
This guide breaks down chest pain in practical terms, helping you recognize when it’s serious, how it’s diagnosed, and what treatment options are available through modern cardiac services.
What Is Chest Pain, Really?
Chest pain is not a diagnosis. It’s a symptom—and one that can originate from several different systems in the body.
Patients describe it in many ways:
- Tightness or pressure
- Sharp or stabbing pain
- Burning or aching
- A feeling of heaviness or squeezing
It may last seconds or hours. It may spread to the arm, jaw, back, or shoulder. Some people feel it during activity; others at rest.
From a cardiology standpoint, the goal is simple but urgent: determine whether the pain is cardiac or non-cardiac, and act accordingly.
Cardiac Causes of Chest Pain
Coronary Artery Disease (CAD)
Coronary artery disease is the most common and most dangerous cause of cardiac-related chest pain.
It occurs when plaque builds up inside the coronary arteries, restricting blood flow to the heart muscle. When the heart doesn’t get enough oxygen—especially during exertion—it sends a warning signal in the form of chest pain, known as angina.
Typical features include:
- Pressure or squeezing in the center of the chest
- Pain triggered by physical activity or stress
- Relief with rest
Left untreated, coronary artery disease can lead to heart attacks, heart failure, or sudden cardiac death.
Heart Attack (Myocardial Infarction)
A heart attack happens when a coronary artery becomes completely blocked. This is a medical emergency.
Chest pain associated with a heart attack often:
- Feels intense and persistent
- Radiates to the arm, jaw, neck, or back
- Is accompanied by sweating, nausea, or shortness of breath
If chest pain is severe, new, or worsening—do not wait. Emergency care is critical.
Other Heart-Related Causes
Not all cardiac chest pain is due to blocked arteries. Other possibilities include:
- Pericarditis: Inflammation of the sac around the heart
- Aortic dissection: A tear in the aorta, often sudden and severe
- Cardiomyopathy: Thickened or weakened heart muscle
- Arrhythmias: Abnormal heart rhythms causing chest discomfort
Each requires specialized cardiac evaluation and treatment.
Non-Cardiac Causes of Chest Pain
One of the most common misconceptions is that chest pain always equals heart disease. In reality, many cases come from other systems.
Gastrointestinal Causes
Acid reflux and esophageal spasms can closely mimic heart pain. Burning sensations after meals, pain when lying down, or relief with antacids often point to a digestive cause.
Musculoskeletal Pain
Strained chest muscles, rib injuries, or costochondritis can cause sharp, localized pain—often worse with movement or touch.
Lung-Related Conditions
Conditions such as pneumonia, pulmonary embolism, or pleuritis can cause chest pain, especially when breathing deeply.
Anxiety and Panic Disorders
Anxiety-related chest pain is real and distressing. However, it’s a diagnosis made only after cardiac causes are ruled out—not before.
Why Medical Evaluation Matters
The danger with chest pain isn’t just what it is—it’s what it could be.
Many patients hesitate, hoping symptoms will pass. Others assume they’re “too young” or “too healthy” for heart disease. Unfortunately, coronary artery disease does not always announce itself politely.
A thorough cardiac evaluation ensures:
- Life-threatening causes are ruled out
- Appropriate treatment starts early
- Long-term heart damage is prevented
How Cardiologists Diagnose Chest Pain
Detailed Medical History
We start by listening. The quality, duration, triggers, and location of chest pain tell us more than most tests ever could.
Key questions include:
- When did the pain start?
- What makes it better or worse?
- Does it occur with exertion?
- Are there risk factors like diabetes, smoking, or family history?
Physical Examination
Heart sounds, blood pressure, lung function, and signs of fluid retention provide critical clues.
Diagnostic Testing
Depending on findings, diagnostic tests may include:
- Electrocardiogram (ECG): Identifies heart rhythm issues or signs of ischemia
- Blood Tests: Detect markers of heart muscle damage
- Stress Testing: Evaluates blood flow during exertion
- Echocardiogram: Visualizes heart structure and function
- Cardiac CT or Angiography: Identifies blocked arteries
These tools allow cardiologists to confirm or rule out coronary artery disease with precision.
Treatment Options for Chest PaiTreatment depends entirely on the cause.
Treating Coronary Artery Disease
Management often includes:
- Lifestyle modifications
- Cholesterol and blood pressure medications
- Blood thinners
- Minimally invasive procedures such as angioplasty or stenting
Early intervention can dramatically improve outcomes.
Medication Management
For non-emergency cardiac chest pain, medications may include:
- Beta blockers
- Nitrates
- Calcium channel blockers
Each works differently to reduce heart strain and improve blood flow.
Non-Cardiac Treatment
When chest pain isn’t heart-related, treatment may involve:
- Acid suppression therapy
- Physical therapy
- Anxiety management
- Pulmonary care
Even non-cardiac chest pain deserves proper diagnosis—self-treatment can be risky.
The Role of Preventive Cardiac Services
One of the most overlooked aspects of chest pain management is prevention.
Comprehensive cardiac services don’t just treat disease—they help prevent it through:
- Risk assessment
- Advanced imaging
- Lifestyle counselin
- Long-term monitoring
Preventive cardiology is especially important for patients with family history or silent coronary artery disease.
When to Book an Appointment
You should Book an Appointment with a cardiologist if:
- Chest pain is recurrent or unexplained
- Pain occurs during activity
- You have risk factors for heart disease
- Symptoms are worsening or changing
Waiting for symptoms to “go away” can cost valuable time.
Trust, Experience, and Personalized Care
Every patient is different. Chest pain in a 35-year-old athlete doesn’t mean the same thing as chest pain in a 65-year-old with diabetes.
That’s why experience matters.
Cardiology isn’t just about reading test results—it’s about interpreting them in context, recognizing subtle patterns, and making informed decisions that prioritize patient safety.
Final Thoughts
Chest pain should never be ignored, dismissed, or self-diagnosed. Whether it turns out to be muscular strain or coronary artery disease, the only safe path forward is proper evaluation.
Modern cardiac services allow us to diagnose accurately, treat effectively, and—most importantly—prevent future complications.
If you or someone you love is experiencing chest pain, don’t wait for clarity to come on its own. Book an Appointment and take the first step toward answers, reassurance, and heart health.