Chest pain is one of the most alarming symptoms a person can experience. Whether it appears suddenly or develops gradually, chest discomfort often raises immediate concern about the heart—and for good reason. While not all chest pain is life-threatening, some causes require urgent medical attention. Understanding why chest pain happens, how it is diagnosed, and what treatment options are available can empower you to protect your heart health and respond appropriately.
This comprehensive guide explains the common and serious causes of chest pain, how physicians evaluate it, and what modern chest pain treatment looks like today—following evidence-based medical standards and Google’s EEAT (Experience, Expertise, Authoritativeness, Trustworthiness) guidelines.
Understanding Chest Pain: More Than Just the Heart
Chest pain is not a diagnosis—it is a symptom. The chest contains the heart, lungs, esophagus, muscles, ribs, nerves, and major blood vessels. Any of these structures can cause pain, pressure, burning, or discomfort.
Chest pain may feel like:
- Tightness or squeezing
- Sharp or stabbing pain
- Burning or aching
- Pressure or heaviness
- Pain radiating to the arm, neck, jaw, or back
Because symptoms overlap, professional evaluation is essential to determine the underlying cause.
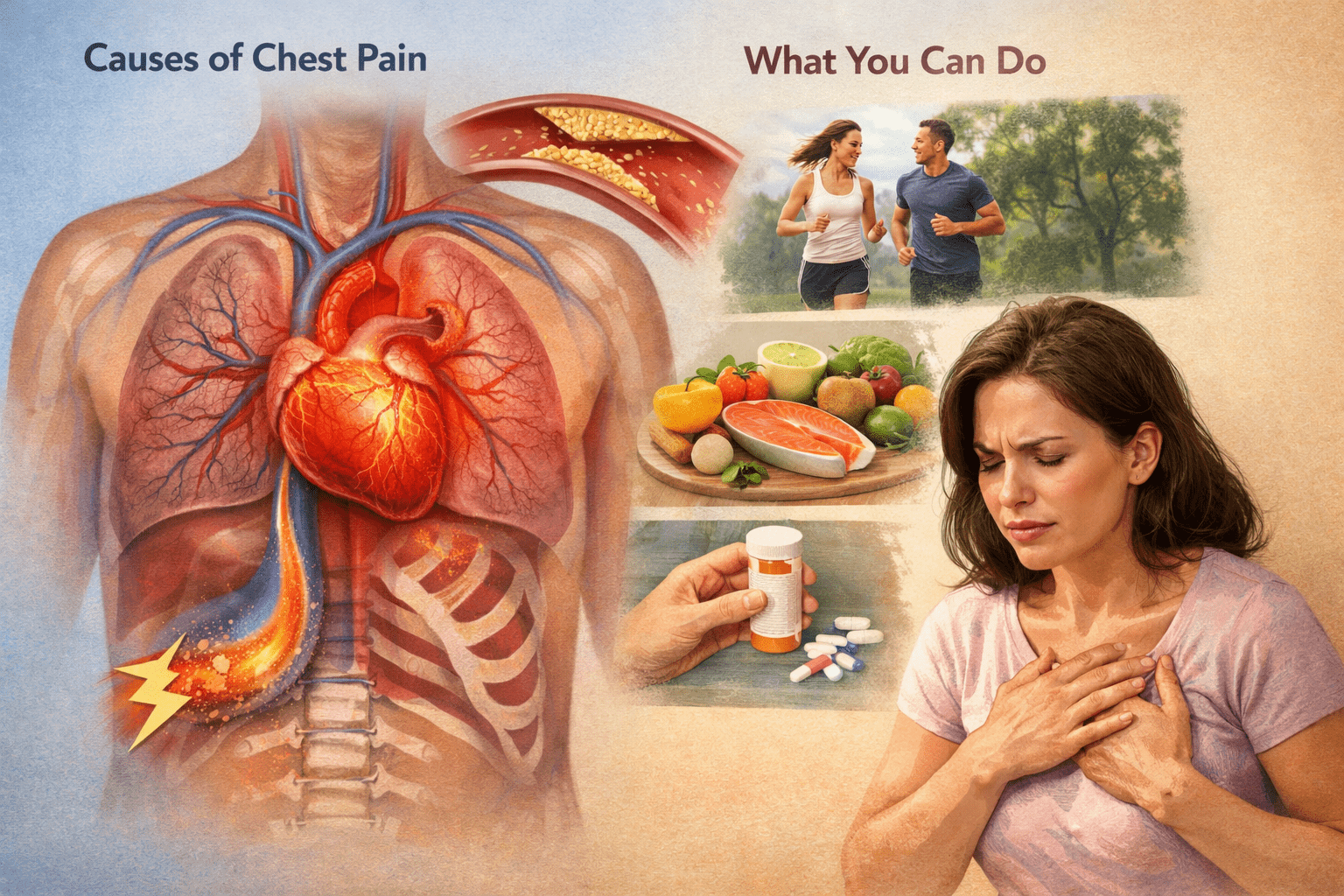
Common Causes of Chest Pain
1. Heart-Related Causes (Cardiac Chest Pain)
Coronary Artery Disease (CAD)
CAD occurs when plaque builds up in the coronary arteries, reducing blood flow to the heart. This often leads to angina, a classic cause of chest pain.
Typical symptoms:
- Pressure or squeezing sensation
- Pain triggered by exertion or stress
- Relief with rest
Heart Attack (Myocardial Infarction)
A heart attack happens when blood flow to part of the heart is completely blocked.
Warning signs include:
- Persistent chest pressure
- Shortness of breath
- Nausea or sweating
- Pain spreading to the arm or jaw
Immediate emergency care is critical.
Congestive Heart Failure
Congestive heart failure occurs when the heart cannot pump blood effectively. While chest pain is not always present, it can occur due to increased strain on the heart or reduced oxygen delivery.
Symptoms may include:
- Chest discomfort
- Fatigue
- Fluid retention
- Shortness of breath
Early detection and management are essential for long-term heart health.
2. Lung-Related Causes
Pulmonary Embolism
A blood clot in the lungs can cause sudden, sharp chest pain that worsens with breathing.
Pneumonia or Pleuritis
Inflammation or infection of the lungs or lung lining can cause localized chest pain, often accompanied by fever or cough.
3. Digestive Causes
Gastroesophageal Reflux Disease (GERD)
Acid reflux is a very common non-cardiac cause of chest pain.
Symptoms often include:
- Burning sensation behind the breastbone
- Pain after eating
- Sour taste in the mouth
GERD-related pain can closely mimic heart pain, making evaluation important.
Esophageal Spasms
These painful contractions can cause severe chest discomfort that feels cardiac in nature.
4. Musculoskeletal Causes
Costochondritis
Inflammation of the cartilage connecting the ribs to the breastbone can cause sharp, reproducible pain.
Muscle Strain or Rib Injury
Physical activity, trauma, or poor posture may lead to chest wall pain.
5. Anxiety and Stress-Related Chest Pain
Panic attacks and chronic anxiety can cause chest tightness, rapid heartbeat, and shortness of breath. Although not physically dangerous, these symptoms should never be assumed to be “just anxiety” without medical evaluation.
When Chest Pain Is an Emergency
Seek immediate medical attention if chest pain:
- Is sudden or severe
- Lasts more than a few minutes
- Occurs with shortness of breath
- Radiates to the arm, jaw, or back
- Is accompanied by nausea, dizziness, or sweating
Prompt diagnosis can be lifesaving.
How Chest Pain Is Diagnosed
Accurate diagnosis is the cornerstone of effective chest pain treatment.
Medical History and Physical Exam
Your doctor will assess:
- Pain characteristics
- Risk factors (smoking, diabetes, high blood pressure)
- Family history of heart disease
Diagnostic Testing
Common tests include:
- Electrocardiogram (ECG) to assess heart rhythm
- Blood tests to detect heart damage
- Chest X-ray to evaluate lungs and bones
- Stress testing to assess blood flow
- Echocardiogram to visualize heart function
- CT scans or coronary angiography for detailed imaging
These tools help differentiate between cardiac and non-cardiac causes.
Chest Pain Treatment Options
Treatment depends entirely on the underlying cause.
Cardiac-Related Chest Pain Treatment
For heart-related conditions, treatment may include:
- Antiplatelet or anticoagulant medications
- Blood pressure and cholesterol management
- Nitroglycerin for angina
- Lifestyle modifications
- Interventional procedures such as stenting or bypass surgery
Patients with congestive heart failure may require:
- Diuretics to reduce fluid overload
- Medications to improve heart function
- Dietary sodium restriction
- Ongoing cardiac monitoring
Non-Cardiac Chest Pain Treatment
Digestive Causes
- Acid-reducing medications
- Dietary changes
- Avoiding trigger foods
Musculoskeletal Causes
- Anti-inflammatory medications
- Physical therapy
- Rest and posture correction
Anxiety-Related Chest Pain
- Stress management
- Cognitive behavioral therapy
- Breathing exercises
- Medication if needed
Protecting Your Heart Health Long-Term
Preventing chest pain starts with proactive heart health strategies:
Lifestyle Changes
- Maintain a balanced, heart-healthy diet
- Exercise regularly
- Quit smoking
- Manage stress
- Maintain a healthy weight
Regular Medical Care
- Monitor blood pressure and cholesterol
- Manage diabetes effectively
- Follow up regularly with your healthcare provider
Early intervention dramatically reduces the risk of serious complications.
Why Medical Expertise Matters
Chest pain should never be self-diagnosed. Board-certified physicians use evidence-based guidelines, advanced diagnostics, and clinical experience to determine the safest and most effective treatment path. This ensures accurate diagnosis, reduces unnecessary anxiety, and protects long-term cardiovascular health.
Final Thoughts
Chest pain is a symptom that demands attention—but not panic. While some causes are benign, others may signal serious heart conditions such as coronary artery disease or congestive heart failure. Understanding the possible causes, seeking prompt evaluation, and following a personalized chest pain treatment plan can make all the difference.
As emphasized by Dr. Cynthia, a trusted medical expert in cardiovascular care, timely diagnosis and evidence-based treatment are essential for protecting long-term heart health. If you or a loved one experiences unexplained chest pain, don’t delay. Early diagnosis, expert care, and preventive strategies form the foundation of a healthier, safer future.