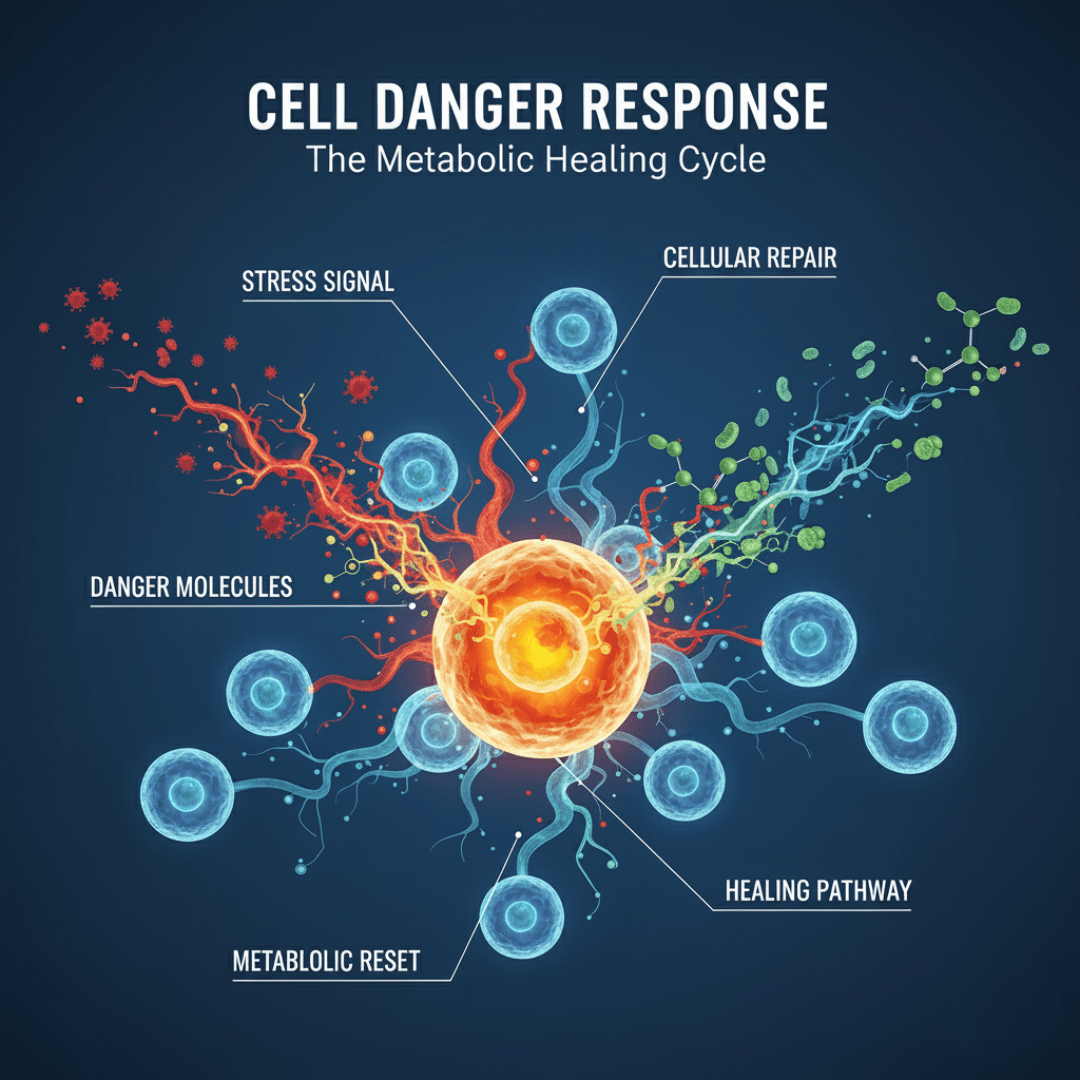
The human body is a marvel of evolutionary engineering, possessing sophisticated defense mechanisms designed to ensure survival against a constant barrage of threats. Among the most fundamental of these systems is the Cell Danger Response (CDR), a universal, evolutionarily conserved metabolic program first described by Dr. Robert Naviaux. The CDR is the cell’s structured and prioritized response to any encounter with chemical, physical, or biological threats—ranging from acute viral infections and environmental toxins to chronic psychosocial stress—that exceed its capacity for normal homeostasis. While fundamentally protective and life-saving in the short term, the pathological persistence of the CDR is increasingly recognized as a central, unifying feature underlying the transition from acute injury to chronic, debilitating disease states, including myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), autism spectrum disorder (ASD), post-traumatic stress disorder (PTSD), and various autoimmune conditions.
The CDR reframes chronic fatigue syndrome not as a failure of the body to respond, but as a state of incomplete healing. It posits that when the danger signals do not fully resolve, cells become metabolically ‘stuck’ in a state of defense, diverting energy and resources away from essential functions like tissue repair, detoxification, and normal immune regulation. This persistent metabolic siege creates a self-sustaining loop of dysfunction that manifests systemically as chronic inflammation, systemic fatigue, and organ-level impairment, offering a novel diagnostic and therapeutic paradigm for complex, multi-system disorders that have historically defied conventional treatment approaches. Understanding the phases and molecular mechanisms of the CDR is crucial for developing targeted interventions aimed at persuading the cell that the danger has passed, thereby enabling the complete restoration of the healing cycle.
This intersection of chronic disease and cellular metabolism helps explain why so many seemingly unrelated disorders share overlapping biochemical patterns—such as mitochondrial dysfunction, oxidative stress, and immune dysregulation. When metabolism is chronically redirected toward defense rather than repair, it disrupts cellular energetics at every level, leading to fatigue, inflammation, and impaired recovery across multiple organ systems, including the heart.
The Sentinel and the Switch: Mitochondria and Metabolic Reprogramming
At the heart of the CDR lies the mitochondrion, famously known as the cell’s powerhouse. However, contemporary research reveals the mitochondria’s function extends far beyond mere energy production; they serve as sentinels that continuously scan the internal and external cellular environment for signs of danger, acting as the “canary in the coal mine” for cellular stress.
When a threat is detected, the mitochondria initiate a rapid and profound shift in cellular bioenergetics—the very mechanism that characterizes the CDR. In a healthy, resting cell (CDR-Safe), energy is generated primarily through oxidative phosphorylation (OXPHOS), a highly efficient process that uses oxygen to create copious amounts of adenosine triphosphate (ATP).
The sudden perception of danger, however, triggers an immediate metabolic switch. The cell deliberately suppresses OXPHOS and reverts to the more ancient and less efficient pathway of glycolysis (the burning of sugar).
This metabolic reprogramming serves a dual purpose: first, it rapidly conserves valuable oxygen and molecular building blocks (such as lipids and nucleotides) to prevent their capture and use by an invading pathogen, effectively starving the enemy. Second, it shifts the function of the remaining mitochondria away from producing high-energy currency (ATP) and toward synthesizing metabolic intermediates.
These intermediates are urgently needed for defensive actions, including the synthesis of reactive oxygen species (ROS) for antimicrobial defense, and the stiffening of the cell membrane to contain damage and prevent the spread of infection. This strategic metabolic mismatch—between available resources and the functional capacity required for normal daily operations—is the defining signature of the acute CDR.
In chronic disease and cellular metabolism dysregulation, this mismatch becomes long-term. Mitochondria remain trapped in defense mode, resulting in persistent fatigue, oxidative stress, and reduced cardiac resilience. This connection between mitochondrial signaling and cardiac metabolism is an emerging focal point in understanding why certain patients develop chronic cardiovascular dysfunction even after the initial injury or inflammation resolves.
The Healing Cycle: Three Choreographed Stages of Recovery
Dr Cynthia Thaik conceptualized the CDR as a programmed, three-stage healing cycle, each step requiring the cell to pass a key metabolic checkpoint (CP) to progress toward full recovery. When the CDR persists pathologically, it means the cell has become locked at one of these stages, unable to signal ‘safety’ and move forward.
Stage 1: CDR1—Defense and Containment
The first phase, CDR1, is the acute response to injury or threat. It is characterized by an extreme shift to glycolysis and maximum deployment of defense mechanisms.
- Key Function: Detects invaders, contain damage, and activate innate immunity.
- Metabolic Signature: Glycolysis dominates; OXPHOS is suppressed.
- Mitochondrial Status: Mitochondria shift from the resting M2 phenotype (filamentous, OXPHOS-optimized) to tWhe M1 phenotype (pro-inflammatory, defense-focused).
- Signaling: Massive release of extracellular ATP (eATP). eATP acts as a purinergic “danger signal,” informing neighboring cells of the threat and driving systemic responses like pain, inflammation, and fatigue (a conserved, adaptive behavior to force rest and recovery).
- Resolution Checkpoint (CP1): Requires the neutralization and clearance of the initial threat (e.g., pathogen elimination, toxin removal). Failure to clear the threat or its residual damage locks the cell into chronic inflammation.
Stage 2: CDR2—Repair and Regeneration
If CP1 is cleared, the cell enters the CDR2 phase, focusing on cellular rebuilding.
- Key Function: Repair damaged tissue and replace lost cells, involving cellular proliferation and differentiation.
- Metabolic Signature: Aerobic glycolysis (a form of the Warburg effect) is prominent. The cell uses glucose and oxygen to produce cellular building blocks (lipids, amino acids, nucleotides) rather than just ATP.
- Mitochondrial Status: Recruitment of M0 mitochondria (undifferentiated, pro-proliferative) from neighboring stem cells to help build new tissue and organelles.
- Resolution Checkpoint (CP2): Requires successful tissue replacement, remodeling, and a metabolic shift away from uncontrolled proliferation. Failure here can lead to pathological tissue remodeling, fibrosis, or unchecked cell growth.
Stage 3: CDR3—Restoration and Connection
The final phase is the return to normal function and specialized cellular identity.
- Key Function: Stop proliferating, differentiate back into specialized cells (e.g., neuron, hepatocyte), reconnect with neighboring cells, and restore efficient energy production.
- Metabolic Signature: Autonomous OXPHOS is fully restored; eATP levels drop to resting values.
- Mitochondrial Status: Dominance of the healthy M2 phenotype (filamentous, pro-homeostatic, anti-inflammatory).
- Resolution Checkpoint (CP3): Signaling pathways confirm the environment is safe, leading to the full resolution of inflammation and the return to health and optimal system performance. Persistent danger signals block CP3, resulting in chronic hypometabolic states like ME/CFS.
The Molecular Toolkit of Defense and Dysfunction
The cellular defense strategy involves several critical molecular players that are co-opted or amplified during the CDR:
- Extracellular ATP (eATP) and Purinergic Signaling: ATP, normally the cell’s energy currency, becomes an essential danger-associated molecular pattern (DAMP) when released outside the cell. High levels of eATP are the definitive signal of danger, binding to purinergic receptors (P2X, P2Y) on the surface of immune and glial cells, driving the inflammation, pain, and fatigue characteristic of CDR1. Persistent eATP signaling acts as a brake on healing, actively suppressing mitochondrial function and inhibiting the progression through the healing cycle.
- Reactive Oxygen Species (ROS): Often considered harmful, ROS are strategically produced during the CDR as necessary signaling molecules and chemical weapons. They contribute to the oxidative environment needed to kill invading microbes. However, if the CDR persists, the chronic elevation of ROS can lead to widespread oxidative damage, particularly to the vulnerable lipid molecules within cell and mitochondrial membranes, further compromising cellular function and perpetuating the danger signal.
- Membrane Stiffening and Lipid Dynamics: The cell membrane undergoes a defensive reinforcement phase, becoming more rigid and less permeable. This limits the entry of pathogens and toxins but also impairs critical communication and transport processes (like hormone signaling and nutrient uptake). The integrity and fluidity of these membranes, which are highly dependent on healthy phospholipids and balanced fatty acids (e.g., Omega-3s), are critical checkpoints for resolving the CDR. Damage to these membranes by oxidized lipids (e.g., malondialdehyde) creates a continuous danger signal, anchoring the cell in survival mode.
- Vitamin D and Immune Dysregulation: The CDR actively disrupts normal Vitamin D metabolism. Mitochondrial P450 enzymes responsible for activating Vitamin D are suppressed, while enzymes that inactivate it are upregulated. This shift supports the pro-inflammatory state of CDR1 and CDR2, suggesting that seemingly unrelated systemic issues like Vitamin D deficiency may actually be part of the cell’s active, programmed defense response, contributing to chronic immune system dysfunction.
The Persistent CDR – The Root of Chronic Fatigue Syndrome
In an ideal scenario, the healing cycle runs its course, the threat is neutralized, and the cell returns to CDR-Safe. However, chronic illness is believed to be the consequence of the CDR becoming abnormally sustained or “stuck.”
This maladaptive persistence is central to both chronic disease and cellular metabolism failure, where the body’s energy production remains hijacked by survival mechanisms. The result is a metabolic gridlock that not only drives chronic fatigue but also impairs cardiac tissue repair, endothelial function, and systemic healing.
- Chronic Low-Grade Toxin Exposure: Continuous exposure to mold toxins, heavy metals, pesticides, or other environmental chemicals acts as a continuous low-level trigger, preventing CP1 resolution.
- Unresolved Chronic Infections: Subclinical viral or bacterial reservoirs (e.g., Borrelia, reactivation of dormant viruses) maintain the immune system in a state of high alert, perpetuating CDR1.
- Oxidative Stress and Membrane Damage: The accumulation of damaged, oxidized lipids in cellular membranes sends non-stop danger signals, which the cell interprets as ongoing physical injury.
- Psychosocial Stress: Chronic psychological trauma, bereavement, or stress are sensed by the brainstem, which is intricately linked to CDR control, leading to systemic activation of the CDR, even in the absence of a biological pathogen.
When the CDR is stuck, the body sacrifices long-term health for short-term survival. Key organs are affected: the brain experiences neuro-inflammation and fatigue (due to constant eATP signaling and low energy), the gut microbiome is disturbed, and detoxification pathways (like bile flow) are suppressed to conserve resources, ironically allowing toxins to accumulate and further fuel the danger signal. The net result is a systemic state of low-grade inflammation, impaired cellular function, and profound energy deficit that characterizes diseases like fibromyalgia, autoimmune disorders, and chronic neurological conditions.
Abating the Danger Signal: The Role of Low-Dose Naltrexone (LDN)
The therapeutic challenge in chronic CDR states is not to treat the symptoms, but to interrupt the pathological feedback loops that keep the healing cycle blocked. One of the most promising and widely discussed tools in this emerging field is Low-Dose Naltrexone (LDN). Naltrexone is a non-selective opioid receptor antagonist typically used at high doses (50mg+) to treat opioid and alcohol dependence. However, at ultra-low doses (usually 1.5mg to 4.5mg), its mechanism of action fundamentally shifts. LDN provides a transient blockade of opioid receptors, which triggers a compensatory rebound in the production of endogenous opioids, such as Opioid Growth Factor (OGF) and its receptor (OGFr). OGF is a potent natural regulator of cell proliferation and is generally anti-inflammatory. More critically in the context of CDR, LDN exerts a powerful immunomodulatory and anti-inflammatory effect by antagonizing Toll-Like Receptor 4 (TLR4), a critical sentinel protein on immune cells (microglia, astrocytes, macrophages) that responds to pathogens and DAMPs. By inhibiting the chronic overactivation of TLR4, particularly on microglial cells in the central nervous system, LDN effectively dampens the excessive release of pro-inflammatory cytokines (like TNF-$\alpha$ and IL-6) that are characteristic of the prolonged CDR state. Furthermore, LDN can influence macrophage polarization, promoting the shift from the pro-inflammatory M1 phenotype (CDR1) towards the restorative M2 phenotype (CDR3), thereby assisting the cell in resolving inflammation and re-entering the repair phase. By calming neuro-inflammation and modulating the core immune-metabolic signaling pathways that maintain the CDR, LDN helps to “turn down the volume” on the pervasive cellular danger signals, allowing the body’s natural healing mechanisms to take over and progress the stalled CDR cycle toward resolution.
By calming neuroinflammation and modulating the core immune-metabolic signaling pathways that maintain the CDR, LDN helps to “turn down the volume” on the pervasive cellular danger signals, allowing the body’s natural healing mechanisms to take over and progress the stalled CDR cycle toward resolution.
In emerging studies, similar metabolic modulation shows promise for cellular healing and heart failure recovery, suggesting that targeting mitochondrial inflammation may become a novel adjunct therapy in precision cardiology.
Conclusion and the Future of Metabolic Medicine
The Cell Danger Response offers a profoundly new lens through which to view the landscape of chronic illness. It moves the conversation away from disease-specific pathogenesis (what caused the injury) and toward the universal mechanisms of salugenesis (how the body achieves health and recovery). The CDR highlights that many seemingly disparate chronic conditions—from neurological disorders to chronic pain and fatigue—share a common final pathway of metabolic dysfunction: a cell defensively stuck in survival mode.
Therapeutic strategies targeting the CDR must focus on two central goals: first, removing the maintaining causes (detoxification protocols to clear chemical triggers, antimicrobial treatments for stealth infections, and trauma-informed stress reduction) and second, restoring cellular health and communication (using tools like LDN to modulate inflammation, replenishing cell membrane lipids, and promoting mitochondrial biogenesis). By understanding the specific metabolic phase in which a patient is stuck, clinicians can apply precise interventions to guide the cell through the checkpoints of the healing cycle. The CDR is not just a scientific model; it is a foundational framework for the future of precision metabolic medicine, offering genuine hope for resolving the rising tide of chronic, multi-system disorders.