
Navigating POTS Syndrome, POTS Heart Disease, and Connection with MCAS:
Find a POTS heart disease syndrome specialist in Burbank Los Angeles CA. Dr. Thaik is a POTS disorder symptoms and adrenal fatigue pots disorder symptoms specialist. For most people, standing up is a natural and effortless part of daily life. But for people affected by a disorder called postural orthostatic tachycardia syndrome (POTS), the simple act of standing can provoke lightheadedness and a racing heartbeat. Postural Orthostatic Tachycardia Syndrome (POTS Disorder Symptoms) is a complex condition that affects millions of people worldwide. It is estimated that pots symptoms affected approximately 3 million Americans before COVID-19. Recent research shows that the number of POTS symptoms patients is now estimated to impact at least 6 million Americans since the pandemic began. While anyone can develop POTS symptoms, approximately 75% of those diagnosed are women between the ages of 15 and 50. POTS symptoms can be triggered by a variety of life stressors including pregnancy, major surgery, trauma, or a viral infection like mononucleosis, Lyme disease, or COVID-19.
POTS is a type of dysautonomia, which means that the autonomic nervous system, responsible for controlling vital functions such as heart rate, blood pressure, and breathing, does not function properly. As a holistic cardiologist practicing in Los Angeles, Dr. Cynthia Thaik, MD, and the staff at Holistic Healing Heart Center have seen many patients with adrenal fatigue POTS. We believe in taking a whole-body approach to evaluating adrenal fatigue POTS or POTS patients and helping patients achieve optimal health and wellness.
Postural Orthostatic Tachycardia Syndrome | POTS Disorder Symptoms
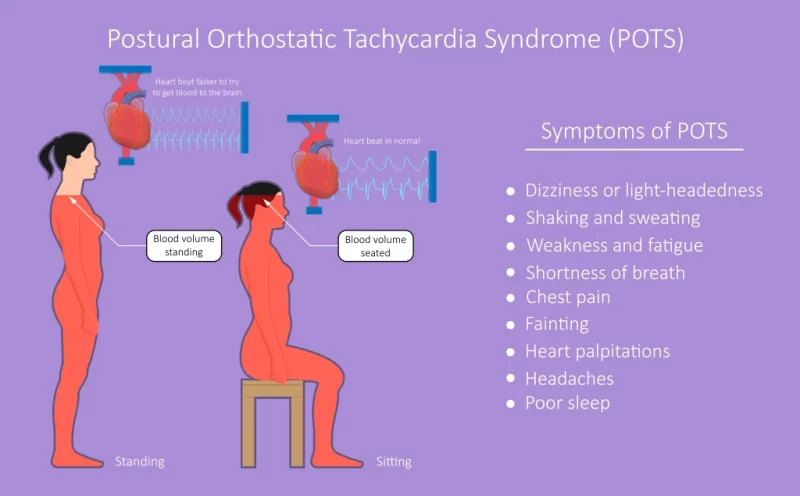
Postural orthostatic tachycardia syndrome (POTS Disorder Symptoms) is one of a group of disorders that have orthostatic intolerance (OI) as their primary symptom of pots heart disease. OI is a condition in which an excessively reduced volume of blood returns to the heart after an individual stands up from a lying down position. Normally, when you stand up, your blood vessels tighten to help pump blood to your brain and other organs. But in people with OI, this doesn’t happen properly, and blood may not reach the brain as efficiently, causing a range of symptoms. Some of the most common symptoms of OI include dizziness, lightheadedness, fatigue, brain fog, palpitations, and sometimes even fainting. OI can be caused by a variety of factors, such as dehydration, low blood pressure, nervous system disorders, and certain medications. Let’s review the definition of POTS. Each word of “postural orthostatic tachycardia syndrome” has a meaning:
- Postural: Related to the position of your body. In POTS Disorder Symptoms are often triggered by changes in position, such as standing up.
- Orthostatic: Related to standing upright. People with POTS often experience symptoms related to standing or sitting up for long periods.
- Tachycardia: A heart rate over 100 beats per minute. In POTS, the heart rate may increase excessively and rapidly upon standing or changing positions.
- Syndrome: A group of symptoms that happen together. POTS is a syndrome that includes a range of symptoms related to the cardiovascular and nervous systems, including rapid heartbeat, lightheadedness, fatigue, and other symptoms that can significantly impact the quality of life.
- A specific group of symptoms that frequently occur when standing upright.
- A heart rate increase from horizontal to standing (or as tested on a tilt table) of at least 30 beats per minute in adults, or at least 40 beats per minute in adolescents, measured during the first 10 minutes of standing.
Postural Orthostatic Tachycardia Syndrome (POTS) is a complex POTS Heart Disease disorder affecting the autonomic nervous system, leading to symptoms such as rapid heart rate, lightheadedness, and fatigue upon standing. Dr. Cynthia delves into the intricacies of POTS, offering clarity on its diverse manifestations and the challenges involved in diagnosis.
Who Does POTS Impact?
POTS predominantly affects women and individuals assigned female at birth, particularly those aged between 15 and 50 years. However, it’s important to note that men and individuals assigned male at birth can also be diagnosed with POTS.
Certain stressors can increase the likelihood of developing POTS, including:
- Significant illnesses, such as viral infections like mononucleosis or severe infections.
- Pregnancy.
- Physical trauma, such as a head injury.
- Surgical procedures. Individuals with specific autoimmune conditions, such as Sjogren’s syndrome, lupus, and celiac disease, are also more prone to developing POTS.
There is new evidence that COVID-19 may trigger POTS, according to data on nearly 300,000 patients from the Cedars-Sinai Health System in Los Angeles County from 2020 to 2022 who had either received at least one dose of a COVID vaccine or had a confirmed case of COVID. While the researchers found a small but increased risk of POTS following COVID vaccination and, in particular, the first dose, the risk was greater following a COVID infection itself: Getting COVID-19 was linked to a five times greater risk of POTS than vaccination.
As a seasoned holistic cardiologist, Dr. Cynthia Thaik elucidates the interplay between POTS syndrome and heart health. The guide explores how POTS can influence cardiovascular function, emphasizing the importance of a holistic approach in managing symptoms and mitigating potential risks to heart well-being.
History of POTS:
The term “POTS” was coined in 1993 by a team of researchers from Mayo Clinic, led by neurologist Dr. Philip Low. However, POTS is not a new illness; it has been known by other names throughout history, such as DaCosta’s Syndrome, Soldier’s Heart, Mitral Valve Prolapse Syndrome, Neurocirculatory Asthenia, Chronic Orthostatic Intolerance, Orthostatic Tachycardia and Postural Tachycardia Syndrome, adrenal fatigue POTS Syndrome.
There is some evidence to suggest that POTS and anxiety can be related, as both conditions can involve similar symptoms such as palpitations, dizziness, and shortness of breath.
POTS Disorder Symptoms:
POTS can manifest suddenly or develop gradually, and its classification is a topic of ongoing discussion. However, most authorities recognize distinct characteristics of POTS Disorder Symptoms, with variations among patients such as adrenal fatigue POTS syndrome symptoms.
Symptoms typically arise immediately or a few minutes after sitting up or standing, with some relief experienced when lying down. The range of symptoms associated with POTS is diverse and varies from person to person, including:
POTS has several possible symptoms, and they vary from person to person. Symptoms include:
- Dizziness or lightheadedness, especially upon standing, prolonged standing, or during extended walks.
- Fainting or near-fainting episodes.
- Disrupted sleep due to chest pain, a racing heart rate, and excessive sweating.
- Forgetfulness and difficulty focusing (brain fog).
- Heart palpitations or a rapid heart rate.
- Exhaustion and fatigue.
- Feelings of nervousness or anxiety.
- Shakiness and excessive sweating.
- Shortness of breath (dyspnea).
- Chest pain.
- Headaches.
- Nausea.
- Bloating.
- Pallor and purple discoloration of hands and feet when positioned below the heart.
- Warm environments, such as hot baths, showers, or on hot days.
- Frequent standing, such as waiting in line or shopping.
- Strenuous exercise.
- Illness, such as a cold or infection.
- Menstruation.
Although the origin of POTS symptoms is physical, sometimes people attribute the symptoms incorrectly to psychological disorders such as anxiety. While some people with POTS Disorder Symptoms have anxiety disorders similar to the general population, POTS is not caused by anxiety.
How Is POTS Diagnosed?
Diagnosis of POTS will generally begin with the physician taking a medical history and performing a physical exam. During the physical exam, the physician may perform a tilt table study to evaluate the heart and blood pressure when the body changes positions. Based on the tilt table test and the patient’s symptoms, an accurate diagnosis can often be made.
In some instances, the physician may order additional tests to rule out other conditions. These diagnostic tests may examine the heart muscle, the blood flow through the heart, and any potential abnormal electrical impulses. An electrocardiogram (EKG) is a painless procedure that provides a picture of the electrical activity of the heart and how the heart is working.
Another diagnostic tool that could be used is an echocardiogram test. This non-invasive procedure uses a machine called a transducer that transmits sound waves and bounces them off the heart and back into the transducer.
Electrophysiology studies may also be used to look at the electrical system of the heart. Your healthcare provider might recommend additional tests to either validate a POTS diagnosis or eliminate other potential causes of your symptoms. These tests may include:
- Blood and urine tests to identify underlying causes of POTS or conditions that mimic its symptoms.
- TST (Tuberculin Skin Test).
- QSART (Quantitative Sudomotor Axon Reflex Test), measuring autonomic nerves controlling sweating.
- Skin nerve biopsy.
- Autonomic breathing test, evaluating your blood rate and pressure response during exercise.
- Echocardiogram.
- Blood volume assessments with hemodynamic studies.
POTS Syndrome Treatments:
Healthcare providers use several strategies to manage the symptoms of POTS. POTS Syndrome Treatment is highly individualized based on your symptoms and what works best for you. The main forms of treatment include:
- Exercise and physical activity: Studies show that reclined aerobic exercise, such as swimming, rowing and recumbent bicycling, has the best results. Strengthening your core and leg muscles is also helpful.
- Diet and nutrition: If you have the hypovolemic (low blood volume) form of POTS, your healthcare provider will likely recommend increasing both your fluid and salt intake to increase blood volume. Eating a large meal can make symptoms of POTS worse, as your body redirects a lot of blood to aid in the digestion process. Because of this, providers often recommend eating several smaller meals throughout the day instead of two or three large ones.
Medical compression stockings can also help push blood up from your legs to reduce POTS symptoms. They may also give you more endurance to tolerate longer amounts of upright activity before your dysautonomia symptoms set in.
Postural Orthostatic Tachycardia Syndrome (POTS) can be a challenging and debilitating condition for those who experience it. However, it is important to be hopeful and recognize that there are treatment of pots options available that can greatly improve quality of life.
With proper treatment of pots disease, many people with POTS are able to manage their symptoms and live fulfilling lives. This can include lifestyle changes such as increasing fluid and salt intake, exercise, and medications such as beta-blockers or midodrine.
POTS vs. Hypermobile Ehlers-Danlos syndrome (EDS) and Hypermobility Spectrum Disorders:
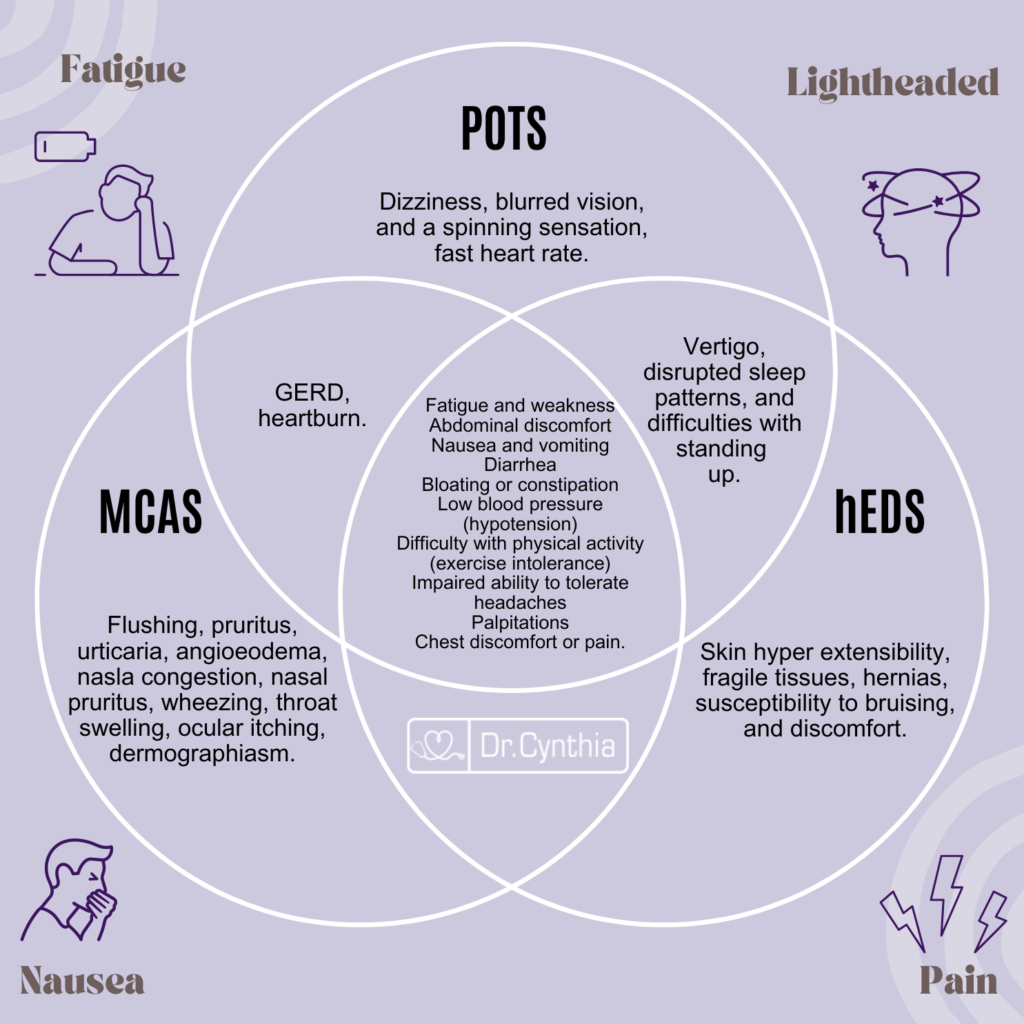
Some of the symptoms of POTS overlap with symptoms of EDS and HSD. Ehlers-Danlos syndrome is a group of disorders that mostly affect your skin, joints, and blood vessels. People with EDS often have very flexible joints and stretchy skin that bruises easily. According to Standing up to POTS, 80% percent of people with Ehlers-Danlos Syndrome have POTS, and most people with POTS have Type III EDS which is the hypermobility type.
Common symptoms of POTS, Hypermobility Spectrum Disorders (HSD), and Hypermobile Ehlers-Danlos Syndrome (EDS) can vary, but there can be some overlapping symptoms, especially between POTS and joint hypermobility-related conditions.
Here are some common symptoms that may be present in patients with EDS and POTS:
- Lightheadedness or Dizziness: Individuals with both POTS and HSD/EDS may experience lightheadedness or dizziness, especially when transitioning from sitting or lying down to a standing position. This symptom often results from orthostatic intolerance.
- Tachycardia (Rapid Heart Rate): Tachycardia, characterized by a rapid heart rate, is a hallmark symptom of POTS. In some cases, individuals with HSD/EDS may also experience an elevated heart rate, especially upon standing or during physical activity, due to autonomic dysfunction.
- Fatigue: Fatigue is a common symptom in both POTS and HSD/EDS. Individuals with either condition may experience profound fatigue, which can significantly impact their daily functioning.
- Joint Hypermobility: is a feature of HSD and hypermobile EDS. While it’s not a primary symptom of POTS, it can sometimes be present in individuals with POTS, especially those with joint hypermobility-related conditions.
- Chronic Pain: Chronic musculoskeletal pain is frequently reported by individuals with HSD/EDS and can also be a symptom in some POTS patients, particularly if they have underlying joint or connective tissue issues.
- Autonomic Dysfunction, which affects the autonomic nervous system responsible for regulating functions like heart rate, blood pressure, and digestion, can be present in both conditions. This dysfunction can contribute to symptoms such as sweating abnormalities, digestive issues, and temperature regulation problems.
- Gastrointestinal Symptoms: Gastrointestinal problems, including abdominal pain, bloating, and irritable bowel syndrome (IBS)-like symptoms, can be seen in both conditions due to autonomic dysfunction.
Mast Cell Activation Syndrome and POTS:
There is a growing awareness in the medical and patient community that some patients with POTS also have mast cell activation syndrome (MCAS). Mast Cell Activation Syndrome (MCAS – also known as Mast Cell Activation Disorder) is a complex and often underdiagnosed condition where mast cells, a type of white blood cell involved in the immune system, become overly activated, releasing an excessive amount of chemical mediators, such as histamine. This can lead to a wide range of symptoms affecting multiple organ systems. MCAS patients experience repeated episodes of the symptoms of anaphylaxis – allergic symptoms such as hives, swelling, low blood pressure, difficulty breathing and severe diarrhea. High levels of mast cell mediators are released during those episodes.
MCAS and POTS can sometimes co-occur in individuals, leading to a more complex clinical picture. The exact relationship between the two conditions is not fully understood, but it’s thought that mast cell activation may contribute to autonomic dysfunction seen in POTS. According to a study published in the Journal of the American Heart Association, MCA disorder is relatively common in patients diagnosed with POTS and who present with additional nonorthostatic gastrointestinal, cutaneous, and allergic symptoms.
Some of the overlapping symptoms of POTS and MCAS include:
- Orthostatic Intolerance: Both POTS and MCAS can lead to orthostatic intolerance, where individuals experience symptoms when transitioning from sitting or lying down to a standing position. Common orthostatic symptoms include lightheadedness, dizziness, and sometimes fainting (syncope).
- Tachycardia (Rapid Heart Rate): Rapid heart rate is a hallmark symptom of POTS. In MCAS, when mast cells release chemical mediators like histamine, it can also lead to tachycardia. Therefore, elevated heart rate can be a shared symptom.
- Gastrointestinal Symptoms: Both conditions can result in gastrointestinal symptoms such as abdominal pain, nausea, diarrhea, and sometimes vomiting. These symptoms can be due to autonomic nervous system dysfunction in POTS or mast cell activation in MCAS.
- Fatigue: Fatigue is a common complaint in both POTS and MCAS. It can be disabling and significantly impact daily functioning.
- Headaches: Headaches, including migraines, can occur in both conditions. These headaches may be related to blood pressure and blood flow changes seen in POTS or mast cell activation in MCAS.
- Brain Fog: Cognitive difficulties, often described as “brain fog,” can be experienced by individuals with both POTS and MCAS. This can include difficulty concentrating, memory problems, and reduced mental clarity.
- Sweating Abnormalities: Sweating abnormalities, such as excessive sweating or changes in body temperature regulation, can occur in both conditions.
- Palpitations: Awareness of heartbeats or palpitations can be reported by individuals with both POTS and MCAS.
Mast Cell Activation Syndrome (MCAS) is a condition characterized by the abnormal activation of mast cells, leading to a cascade of symptoms. Dr. Cynthia explores the intriguing connection between POTS and MCAS, shedding light on how these conditions may coexist and impact each other. This comprehensive exploration provides valuable insights for individuals navigating the complex landscape of overlapping syndromes.
For patients suffering from POTS (Postural Orthostatic Tachycardia Syndrome), MCAS (Mast Cell Activation Syndrome), or Ehlers-Danlos Syndrome (EDS), it’s important to know that you are not alone, and there is hope for managing and improving your quality of life. Finding an understanding and empathetic physician can be a pivotal point on your journey to health and wellness. Dr. Cynthia Thaik and her nutritionist have experience diagnosing and addressing the symptoms related to these two conditions which will help to mitigate the symptoms of POTS.
Patients with POTS Find Support At The Holistic Healing Heart Center In Los Angeles:
Dr. Cynthia Thaik, MD, a leading healthcare professional in Los Angeles, is a holistic cardiologist with a distinguished background, having received her training at Harvard. Known for her compassionate approach, Dr. Thaik practices medicine with a heart-centered focus. Her mission is to alleviate stress, fear, and anxiety in her patients, fostering a deep sense of inner calm and peace.
Dr. Thaik goes beyond traditional medical practices, aiming to empower her clients to proactively engage in their journey toward health and healing. Through education and inspiration, she guides individuals to take meaningful steps that contribute to their overall well-being. Dr. Thaik’s dedicated team has successfully assisted thousands of people in transforming their lives by influencing positive changes in their thoughts, emotions, and actions.
If you’ve received a diagnosis of POTS or are currently grappling with symptoms akin to those associated with POTS, schedule a consultation today as your initial step toward taking charge of your cardiovascular health. It’s essential to recognize that POTS is an ongoing condition characterized by fluctuations in symptoms, influenced by various circumstances, some within your control and others not.
It’s crucial to understand that POTS is not classified as a disease and lacks a definitive pots syndrome cure. Instead, its symptoms are to be effectively managed, acknowledging that it often represents a lifelong condition, albeit with the potential for gradual improvement over time. A key aspect of treatment involves coming to terms with the condition, accepting its role in your life, and acquiring the skills to live with and manage its symptoms so that they do not dominate your daily life.
In my approach to treating patients with POTS, I emphasize the importance of minimizing the use of drugs, as they may have the potential to exacerbate the problem or lead to undesirable side effects. It’s important for patients to recognize that achieving a cure is not within the realm of possibility, but my aim is to provide you with a comprehensive understanding of the physiological aspects of the condition and equip you with strategies to effectively manage your symptoms.
Holistic Strategies for Management:
Dr. Cynthia Thaik’s holistic approach to cardiology extends to the management of POTS syndrome and related conditions. The guide outlines holistic strategies that encompass lifestyle modifications, nutritional support, stress management, and innovative therapies to empower individuals on their healing journey.
Patient-Centered Care at the Holistic Healing Heart Center:
At the Holistic Healing Heart Center, patients are at the core of the care paradigm. Dr. Cynthia Thaik and her team prioritize a patient-centered approach, ensuring that individuals receive personalized care that addresses not only the physical aspects of POTS but also the emotional and spiritual dimensions.




