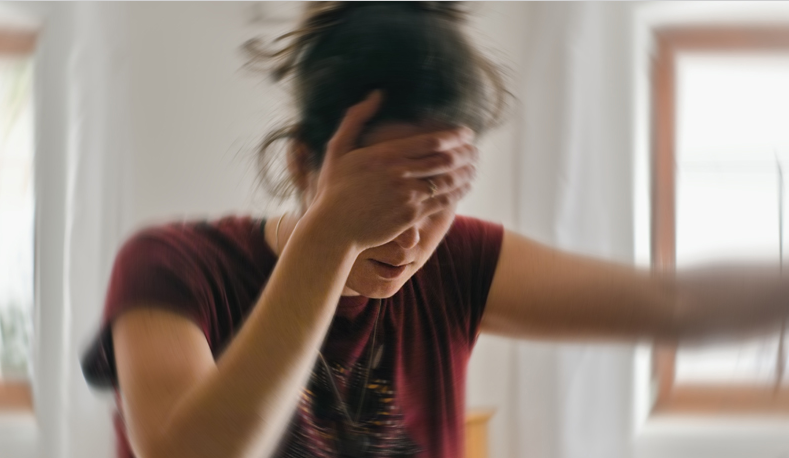
Are you experiencing symptoms like light-headedness, rapid heartbeat, and extreme fatigue? You might be among the millions silently battling with POTS disorder. is a complicated and often misunderstood condition that affects the autonomic nervous system.
In this article, we will unravel the mystery behind POTS disorder, helping you better identify and manage its symptoms. From understanding the underlying causes to exploring various treatment options, we aim to provide you with the knowledge and tools to navigate this silent struggle.
Living with POTS disorder can be challenging, but with the right information and support, you can regain control over your life. Whether you are a patient or a loved one seeking to understand this condition better, this article will serve as a comprehensive guide.
Join us on this informative journey as we shed light on POTS disorder symptoms and empower you with the knowledge to live your life to the fullest. Let us conquer POTS together, one step at a time.
What is POTS disorder?
POTS stands for Postural Orthostatic Tachycardia Syndrome. It is a form of dysautonomia, a disorder of the autonomic nervous system. People with POTS experience a range of symptoms, primarily upon standing, including a rapid heart rate (tachycardia), light-headedness, fainting, and sometimes nausea.
In POTS, there is an abnormal increase in heart rate that occurs when a person stands up. The autonomic nervous system, responsible for regulating various bodily functions, struggles to maintain normal blood pressure and heart rate when transitioning from a seated or lying down position to a standing one. This can lead to the characteristic symptoms associated with POTS.
It’s important to note that POTS is a chronic condition, and its exact cause is often not clear. Symptoms can vary in severity among individuals, and management strategies focus on improving overall quality of life.
Understanding the symptoms of POTS disorder:
Postural Orthostatic Tachycardia Syndrome (POTS) is characterized by a variety of symptoms that primarily occur when a person stands up. While the symptoms can vary from person to person, some common manifestations of POTS include:
- Tachycardia: A rapid increase in heart rate, often exceeding 30 beats per minute within 10 minutes of standing or being upright.
- Light-headedness or Dizziness: Feeling lightheaded, dizzy, or faint upon standing, which may be accompanied by a sensation of unsteadiness.
- Fatigue: Persistent fatigue or exhaustion, which can be debilitating and impact daily activities.
- Weakness: Feeling weak or having difficulty with physical activities, especially when upright.
- Brain Fog: Cognitive difficulties such as difficulty concentrating, memory lapses, and mental fogginess.
- Headaches: Frequent headaches, including migraines, may be associated with POTS.
- Nausea: Feeling nauseous or experiencing abdominal discomfort.
- Exercise Intolerance: Difficulty with physical exertion, often leading to increased symptoms.
- Sleep Disturbances: Problems with sleep, including insomnia or disrupted sleep patterns.
- Palpitations: Awareness of the heartbeat, irregular heartbeats, or a fluttering sensation in the chest.
It’s important to note that POTS symptoms can be triggered or worsened by factors such as heat, dehydration, and prolonged standing. The severity of symptoms can vary, and managing POTS often involves a combination of lifestyle adjustments, medications, and other therapeutic approaches. Individuals experiencing these symptoms should seek medical evaluation for a proper diagnosis and management plan.
The prevalence and impact of POTS disorder:
Postural Orthostatic Tachycardia Syndrome (POTS) is considered a relatively rare disorder, but its prevalence may be underestimated due to underdiagnosis. It often affects young individuals, predominantly women, but can occur in people of any age. The exact prevalence is challenging to determine due to variations in diagnostic criteria and awareness among healthcare providers.
Estimates suggest that POTS may affect tens of millions of individuals globally. The prevalence is higher in certain populations, such as those with chronic fatigue syndrome (CFS) and Ehlers-Danlos syndrome (EDS), indicating a potential association between these conditions.
- Impact of POTS: POTS can have a significant impact on the daily lives and overall well-being of affected individuals. The symptoms, especially the rapid heart rate upon standing, can lead to various challenges:
- Functional Impairment: POTS can limit a person’s ability to engage in routine activities, work, or exercise due to symptoms like dizziness, fatigue, and weakness.
- Reduced Quality of Life: The chronic nature of POTS symptoms can impact emotional well-being and contribute to a lower quality of life.
- Social and Occupational Challenges: Individuals with POTS may face difficulties in social interactions and maintaining employment due to the unpredictable nature of their symptoms.
- Psychological Impact: Living with a chronic condition like POTS can lead to psychological challenges, including anxiety and depression.
- Economic Burden: The financial impact of medical care, medications, and potential disability can pose economic challenges for individuals with POTS and their families.
The prevalence and impact of POTS disorder:

Effective management of POTS involves a multidisciplinary approach, including lifestyle modifications, medications, and targeted therapies. Early diagnosis and appropriate treatment can help improve symptoms and enhance the overall quality of life for those with POTS.
Postural Orthostatic Tachycardia Syndrome (POTS) is a complex disorder that presents challenges in diagnosis due to its diverse symptoms and variable manifestations. While there is no single definitive test for POTS, healthcare professionals employ a combination of clinical evaluation, medical history assessment, and specialized tests to arrive at a diagnosis. Here’s an overview of the diagnostic process for POTS:
Clinical Evaluation
- Detailed Medical History: A comprehensive medical history review is crucial. The healthcare provider will inquire about symptoms, their onset, triggers, and any underlying conditions.
- Physical Examination: A thorough physical examination, including blood pressure measurements, heart rate assessment, and neurological evaluations, helps identify potential signs of POTS.
Symptom Assessment:
Orthostatic Symptoms: POTS is characterized by symptoms that worsen upon standing. Patients may experience light-headedness, palpitations, fatigue, weakness, and difficulty concentrating.
Symptom Diary: Keeping a diary to track symptoms, their intensity, and associated factors provides valuable insights for diagnosis.
Orthostatic Testing:
- Tilt Table Test (TTT): TTT is a standard test for POTS diagnosis. The patient is secured to a table and tilted at different angles while heart rate and blood pressure are monitored.
POTS is often indicated by a significant increase in heart rate without a corresponding drop in blood pressure upon standing.
- Active Stand Test: This simpler test involves measuring heart rate and blood pressure after lying down and standing up.
Blood Tests:
- Autonomic Function Testing: Specific blood tests, such as catecholamine levels, may be conducted to assess the function of the autonomic nervous system.
- Hemodynamic Studies: Hemodynamic studies may evaluate blood volume, cardiac output, and other factors influencing circulation.
Electrocardiogram (ECG or EKG):
- Heart Rhythm Assessment: An ECG helps evaluate the heart’s electrical activity and may reveal any irregularities or arrhythmias.
Holter Monitoring:
- 24-Hour Heart Monitoring: Continuous monitoring over 24 hours using a portable device may capture intermittent heart rate abnormalities not evident during brief clinical assessments.
Autonomic Function Tests:
- Quantitative Sudomotor Axon Reflex Test (QSART): Measures the sweat response to evaluate autonomic function.
- Valsalva Maneuver: Assesses autonomic response to changes in intrathoracic pressure.
Specialized Imaging:
- Magnetic Resonance Imaging (MRI) and Computed Tomography (CT): Imaging studies may be conducted to rule out structural abnormalities or conditions affecting blood flow.
Blood Volume Measurement:
- Red Blood Cell Mass Studies: Some healthcare providers may perform blood volume measurements to evaluate circulatory function.
POTS diagnosis requires a multidisciplinary approach, often involving cardiologists, neurologists, and other specialists. As symptoms and presentations can vary widely, collaboration between healthcare professionals and patients is essential for an accurate diagnosis and effective management.
Managing POTS disorder symptoms through lifestyle changes
Managing Postural Orthostatic Tachycardia Syndrome (POTS) disorder often involves a combination of lifestyle changes to alleviate symptoms and improve overall well-being. Here are key lifestyle adjustments that individuals with POTS may consider:
- Hydration: Maintaining adequate fluid intake is crucial. Increasing salt intake, under the guidance of a healthcare professional, can also be beneficial to support blood volume and circulation.
- Dietary Changes: Adopting a balanced diet can help regulate blood sugar levels and prevent symptoms like dizziness. Small, frequent meals can be more manageable than large meals.
- Compression Garments: Wearing compression stockings or abdominal binders may assist in preventing blood pooling in the lower extremities and alleviate symptoms.
- Elevating the Head of the Bed: Raising the head of the bed by 10 to 20 degrees can help reduce symptoms during sleep and minimize the risk of blood pooling.
- Exercise: A tailored exercise program, prescribed by a healthcare professional, can improve cardiovascular fitness and reduce symptoms. Low-impact exercises, such as swimming or recumbent cycling, are often recommended.
- Cooling Strategies: Heat intolerance is common in POTS. Cooling strategies, such as staying in air-conditioned environments, using cooling vests, or taking cool showers, can help manage symptoms.
- Avoiding Triggers: Identifying and avoiding triggers, such as prolonged standing or hot environments, can minimize symptom exacerbation.
- Salt Loading: Some individuals may benefit from salt-loading strategies, which involve consuming a certain amount of salt daily to support blood volume. However, this should be done under medical supervision.
- Medication Management: Medications, such as beta-blockers, fludrocortisone, or midodrine, may be prescribed to manage symptoms. The choice of medication depends on individual factors and should be determined by a healthcare professional.
- Sleep Hygiene: Ensuring good sleep hygiene practices can contribute to overall well-being. Establishing a regular sleep schedule and creating a comfortable sleep environment are important.
- Stress Management: Stress can exacerbate POTS symptoms. Engaging in stress-reducing activities, such as meditation, deep breathing exercises, or yoga, can be beneficial.
- Orthostatic Training: Gradual exposure to upright positions through a structured orthostatic training program can improve tolerance to standing.
It’s essential for individuals with POTS to work closely with healthcare professionals, including cardiologists, neurologists, and other specialists, to develop a comprehensive management plan tailored to their specific needs. Regular follow-ups and adjustments to the management plan may be necessary based on individual responses and changes in symptoms.
The management of Postural Orthostatic Tachycardia Syndrome (POTS) disorder often involves a combination of medications and treatments aimed at alleviating symptoms and improving overall quality of life. Here are common medications and treatments used for POTS:
- Beta-Blockers: Beta-blockers, such as propranolol or metoprolol, are often prescribed to help control heart rate and reduce palpitations. These medications block the effects of adrenaline on the heart.
- Fludrocortisone: This medication helps increase blood volume by promoting salt and fluid retention. It can be beneficial for individuals with low blood volume.
- Midodrine: Midodrine is a vasoconstrictor that helps raise blood pressure and reduce symptoms like dizziness. It is usually taken before activities that may provoke symptoms.
- Salt Supplements: Some individuals may be advised to increase their salt intake to support blood volume. This is typically done under the guidance of a healthcare professional.
- Ivabradine: This medication lowers heart rate by inhibiting the funny current (If) in the heart’s electrical conduction system.
- Pyridostigmine: Pyridostigmine is sometimes used to improve symptoms by enhancing nerve signals and reducing fatigue.
- Physical Therapy: Exercise and physical therapy, especially programs that focus on cardiovascular fitness and muscle strengthening, can be beneficial. Graded exercise programs are often recommended.
- Occupational Therapy: Occupational therapists can help individuals manage daily activities and provide strategies for energy conservation.
- IV Saline Infusions: Intravenous saline infusions may be administered in severe cases or during acute symptom exacerbations to quickly increase blood volume.
- Compression Garments: Wearing compression stockings or abdominal binders can help prevent blood pooling in the lower extremities and reduce symptoms.
- Cognitive-Behavioral Therapy (CBT): CBT may be used to address anxiety, stress, and coping strategies associated with POTS.
- Lifestyle Modifications: Hydration, dietary changes, elevation of the head of the bed, and avoidance of triggers like heat can play a significant role in symptom management.
- Tilt Table Training: This involves controlled exposure to upright positions to improve tolerance to standing and reduce symptoms.
It is important for individuals with POTS to work closely with a healthcare team, including cardiologists, neurologists, and other specialists, to tailor a treatment plan based on individual needs and responses. Medications and treatments may be adjusted over time, and regular follow-ups are crucial to monitor progress and address any changes in symptoms.
Consultation with Dr. Cynthia Thaik for personalized guidance on managing POTS and optimizing heart health, consider consulting with Dr. Cynthia Thaik. Visit www.drcynthia.com to explore holistic approaches to cardiovascular wellness and schedule a consultation. Incorporating these lifestyle changes, along with medical treatments and interventions, can contribute to better symptom management and an improved quality of life for individuals with POTS. Always consult with healthcare professionals, and for specialized guidance, consider reaching out to Dr. Cynthia Thaik through www.drcynthia.com
Conclusion and Hope for the Future of POTS Disorder Research and Treatment
In conclusion, while Postural Orthostatic Tachycardia Syndrome (POTS) poses unique challenges in diagnosis and management, there is hope on the horizon. Ongoing research, multidisciplinary approaches, and advancements in understanding the underlying mechanisms of POTS are paving the way for more effective treatments and improved patient outcomes.
The journey of individuals living with POTS involves collaboration with healthcare professionals, lifestyle adjustments, and, in some cases, innovative interventions. As we navigate the complexities of this disorder, it’s crucial to acknowledge the resilience and strength of those facing its daily impact. As we move forward, the collaboration between healthcare professionals, researchers, and individuals living with POTS remains paramount. By working together, we can strive towards a future where POTS is better understood, and effectively treated, and where those affected can live fuller, healthier lives.
Hope shines brightly on the horizon, inspiring optimism for breakthroughs in research, increased awareness, and a brighter future for individuals navigating the complexities.