Cholesterol problems may loom large on the horizon, but they need not dictate our fate. Armed with knowledge, determination, and a healthy dose of lifestyle modifications, we can turn the tide against high cholesterol and its associated risks. Let’s heed the warnings whispered by our bodies and embark on a journey towards optimal health—one cholesterol-lowering meal at a time.
In today’s fast-paced world, where convenience often trumps health, it’s easy to overlook the silent threats lurking within our bodies. One such threat is high cholesterol—a condition affecting millions worldwide, silently creeping up and increasing the risk of severe cardiovascular diseases. As we delve into the world of cholesterol, we’ll explore its symptoms, effects, and most importantly, dietary solutions to keep it in check.
Symptoms of Cholesterol Problems:
Cholesterol woes often fly under the radar, with no overt warning signs until it’s too late. However, there are subtle clues the body might throw our way, indicating potential cholesterol issues. Persistent fatigue, frequent chest pains, and shortness of breath could all be red flags waving for attention. Pay heed to numbness or weakness in limbs, as well as sudden dizziness or headaches, as these could be indicative of cholesterol-related complications. Cholesterol problems can often present with subtle symptoms that may go unnoticed until they escalate into more serious health issues. Some common symptoms to watch out for include:
- Persistent fatigue: Feeling unusually tired or lacking energy, even after adequate rest, could be a sign of cholesterol problems.
- Chest pain: Unexplained chest discomfort or pain, especially during physical exertion or stress, should not be ignored and may indicate underlying cholesterol issues.
- Shortness of breath: Difficulty breathing or feeling breathless, particularly during activities that were previously manageable, might signal a cholesterol-related problem affecting heart health.
- Numbness or weakness in limbs: Tingling sensations, numbness, or weakness in the arms or legs could be indicative of reduced blood flow due to cholesterol buildup in the arteries.
- Sudden dizziness or headaches: Episodes of dizziness or headaches, especially if they occur unexpectedly and persistently, warrant attention and evaluation for potential cholesterol-related complications.
- Yellowish deposits around the eyes (xanthelasma): Yellowish patches or bumps that appear on the eyelids or around the eyes could be a visible sign of high cholesterol levels.
- Yellowish lumps on the skin (xanthomas): Raised, yellowish bumps or nodules on the skin, particularly around joints or tendons, may indicate excessive cholesterol levels in the body.
Recognizing these symptoms and seeking medical advice promptly can help diagnose and manage cholesterol problems before they lead to more severe cardiovascular issues.
High Cholesterol Physical Symptoms:
The body has its way of signaling distress, and high cholesterol is no exception. Noticeable physical symptoms might manifest in the form of yellowish deposits around the eyes, known as xanthelasma, or yellowish lumps on the skin, called xanthomas. These visible signs serve as a wake-up call, urging individuals to take proactive measures to manage their cholesterol levels. High cholesterol can manifest in various physical symptoms that may serve as indicators of underlying health issues. Here are some of the physical symptoms associated with high cholesterol:
- Xanthelasma: These are yellowish deposits of cholesterol that build up under the skin, typically around the eyelids. Xanthelasma may appear as small, flat yellowish patches or as raised, yellowish lumps. They are usually painless but can be a visible indication of high cholesterol levels.
- Xanthomas: Similar to xanthelasma, xanthomas are yellowish lumps or nodules that form beneath the skin. They can appear on various parts of the body, including the elbows, knees, hands, feet, and buttocks. Xanthomas are composed of cholesterol and may vary in size and shape.
- Arcus Senilis: Also known as a corneal arcus or arcus lipoides, this is a white or grayish ring that forms around the cornea of the eye. It is caused by the accumulation of cholesterol deposits in the cornea and may be more prominent in individuals with high cholesterol levels, particularly in older adults.
- Tendon Xanthomas: These are cholesterol deposits that accumulate in tendons, causing painless but visible lumps or nodules to form. Tendon xanthomas are most commonly found in the Achilles tendon (at the back of the ankle) and may be associated with conditions such as familial hypercholesterolemia.
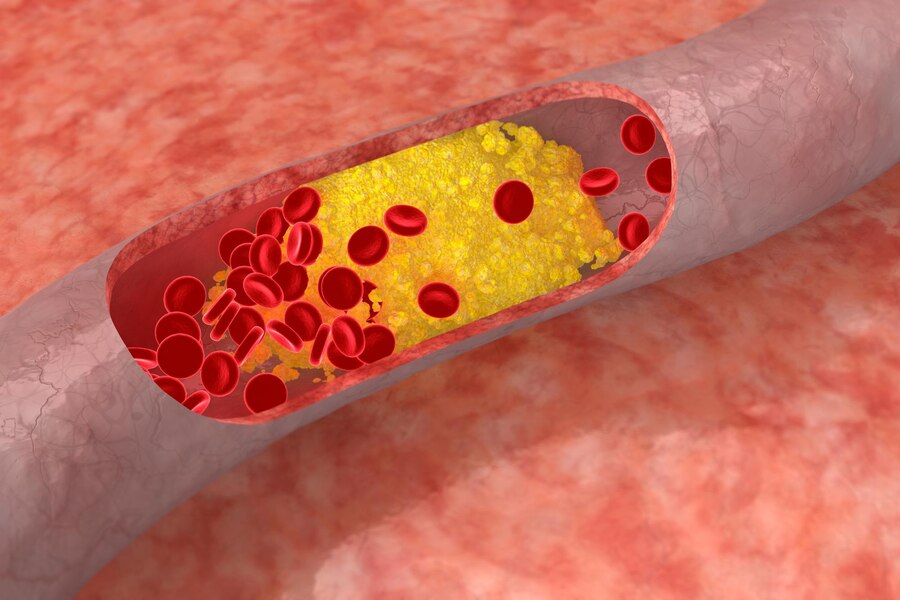
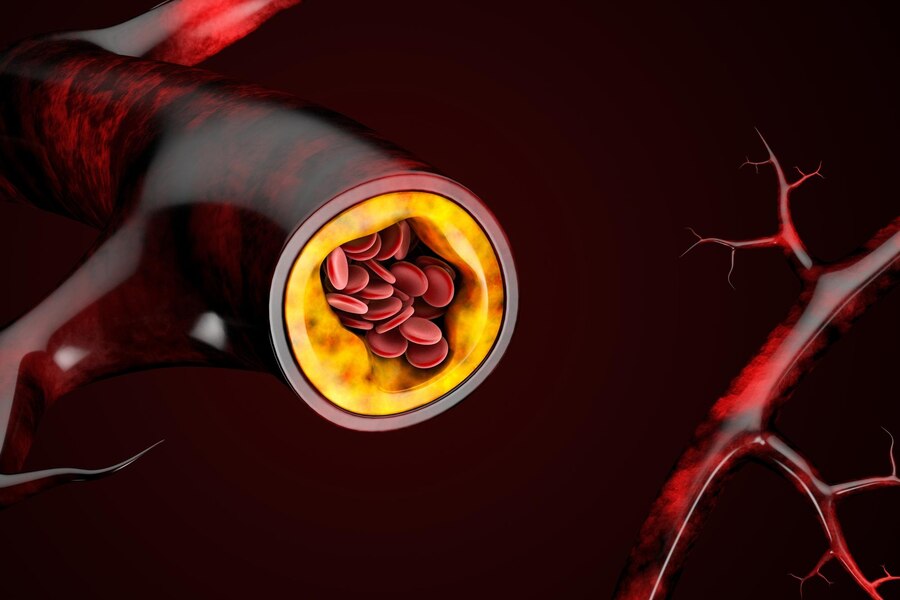
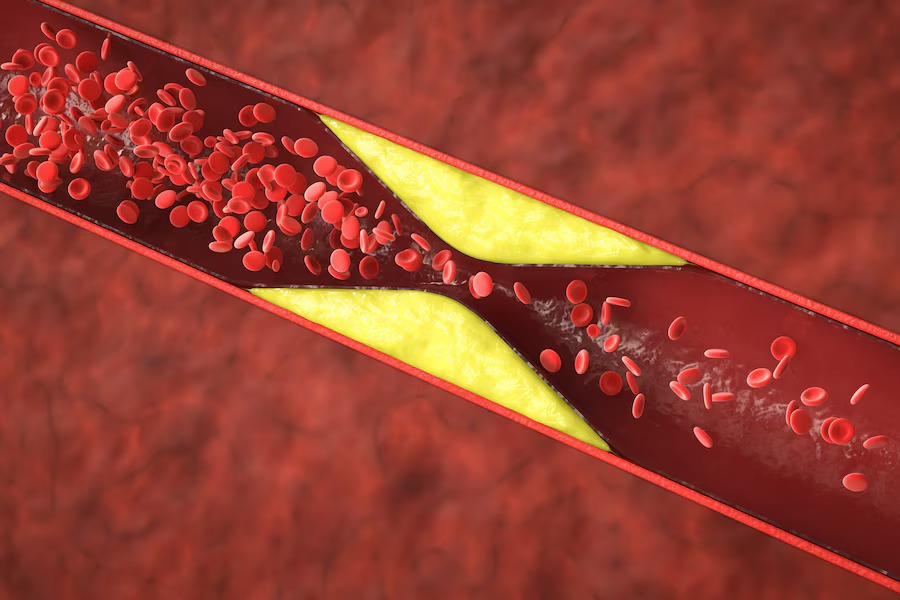
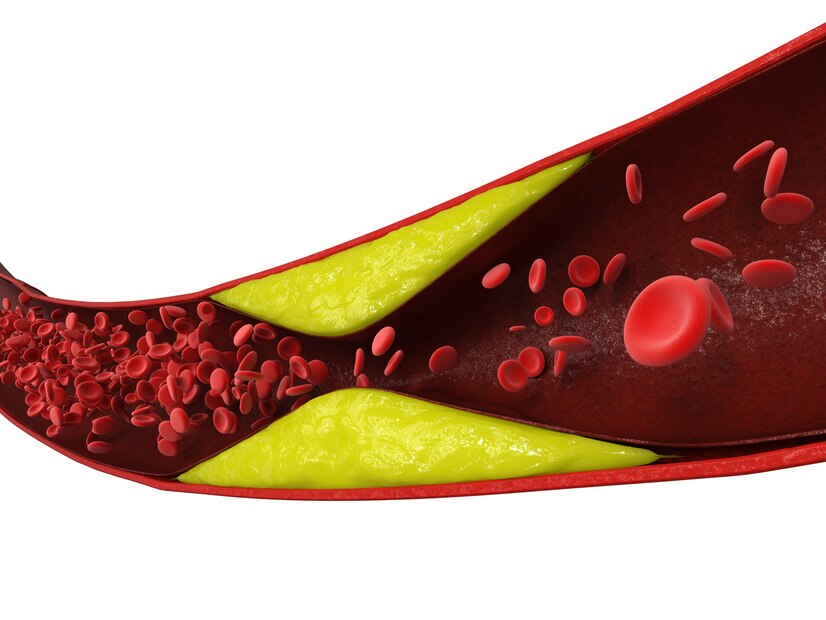
- Cholesterol Deposits in Blood Vessels: High cholesterol levels can lead to the buildup of fatty deposits (plaques) in the walls of blood vessels, a condition known as atherosclerosis. While these deposits may not cause noticeable symptoms initially, they can eventually narrow and block blood flow, leading to complications such as heart disease, stroke, or peripheral artery disease.
Recognizing these physical symptoms of high cholesterol is important for early detection and intervention. Individuals experiencing any of these symptoms should consult with a healthcare professional for proper evaluation and management of their cholesterol levels.
High Blood and High Cholesterol:
High blood pressure and high cholesterol often go hand in hand, forming a deadly duo that wreaks havoc on the cardiovascular system. The arteries, burdened with excess cholesterol, become narrow and stiff, impeding blood flow and increasing blood pressure. This vicious cycle sets the stage for heart attacks, strokes, and other life-threatening conditions. High blood pressure and high cholesterol are two common health conditions that often coexist and contribute to the development of cardiovascular disease. Here’s how they intersect:
- Shared Risk Factors: High blood pressure (hypertension) and high cholesterol (hypercholesterolemia) share many common risk factors, including unhealthy diet, lack of physical activity, smoking, obesity, and genetics. These risk factors can independently and synergistically contribute to the progression of both conditions.
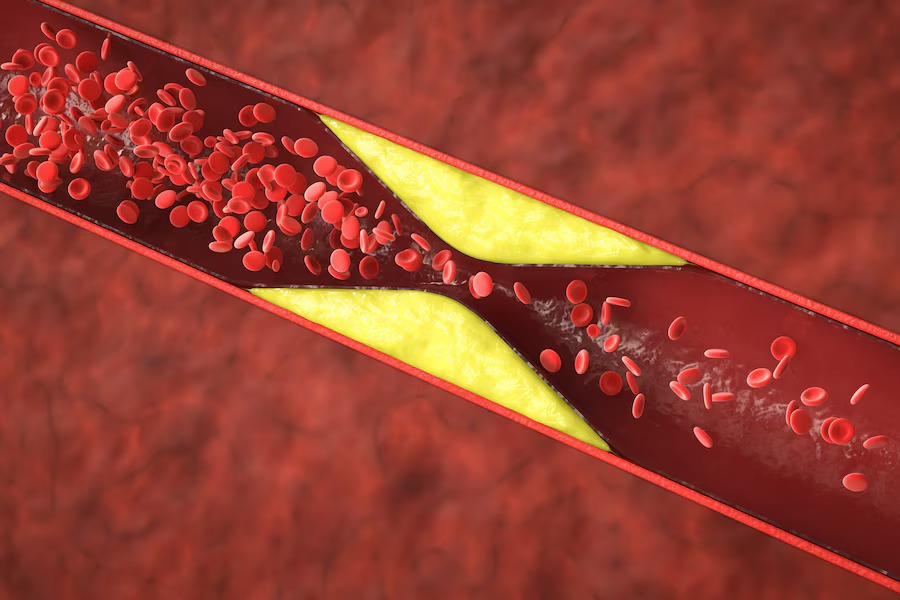
- Effect on Blood Vessels: High blood pressure can damage the walls of blood vessels, making them more susceptible to the buildup of cholesterol-containing plaques. On the other hand, high cholesterol levels can lead to the accumulation of fatty deposits in the walls of blood vessels, narrowing and stiffening them, which can elevate blood pressure.
- Increased Risk of Cardiovascular Disease: When high blood pressure and high cholesterol coexist, the risk of developing cardiovascular disease, including heart attacks, strokes, and peripheral artery disease, is significantly amplified. The combination of elevated blood pressure and cholesterol levels accelerates the progression of atherosclerosis (hardening of the arteries), leading to reduced blood flow to vital organs and tissues.
- Synergistic Effects on Heart Health: Both high blood pressure and high cholesterol impose increased workload and strain on the heart. High blood pressure forces the heart to pump harder to circulate blood through narrowed arteries, while high cholesterol contributes to the formation of plaques that can obstruct blood flow to the heart muscle. This combination can predispose individuals to heart failure, coronary artery disease, and other cardiac complications.
- Treatment Approach: Managing high blood pressure and high cholesterol often requires a multifaceted approach that includes lifestyle modifications and, in some cases, medication. Lifestyle changes such as adopting a heart-healthy diet, engaging in regular exercise, maintaining a healthy weight, quitting smoking, and limiting alcohol intake can help lower both blood pressure and cholesterol levels. Additionally, healthcare providers may prescribe medications such as statins (for cholesterol) and antihypertensives (for blood pressure) to further reduce cardiovascular risk.
Overall, addressing both high blood pressure and high cholesterol is crucial for preserving heart health and reducing the risk of cardiovascular disease. Regular monitoring, lifestyle modifications, and appropriate medical management can help individuals achieve optimal blood pressure and cholesterol levels and mitigate the adverse consequences of these interconnected conditions.

High Blood Lipids Symptoms:
Lipids, including cholesterol, play a crucial role in various bodily functions, but when levels soar, they become a cause for concern. Symptoms such as chest pain, palpitations, and difficulty breathing might signal high blood lipids, prompting individuals to seek medical intervention before irreversible damage occurs. High blood lipids, specifically elevated levels of cholesterol and triglycerides, can have significant implications for cardiovascular health. While high blood lipids often don’t cause noticeable symptoms in the early stages, they can contribute to the development of atherosclerosis (hardening and narrowing of the arteries), which can lead to serious complications such as heart attacks and strokes. However, in some cases, certain signs and symptoms may indicate high blood lipids:
- Xanthomas: These are yellowish, fatty deposits that can develop under the skin, typically on the elbows, knees, hands, feet, or buttocks. Xanthomas may appear as small bumps or nodules and can be a visible sign of high blood lipids.
- Xanthelasma: Similar to xanthomas, xanthelasma are yellowish patches or plaques that form on the eyelids. They are composed of cholesterol deposits and may indicate elevated lipid levels.
- Arcus Senilis: Also known as arcus corneae or corneal arcus, this is a whitish or grayish ring that forms around the cornea of the eye. Arcus senilis is caused by the accumulation of cholesterol in the cornea and may be more common in individuals with high blood lipid levels.
- Pancreatitis: In cases of extremely high triglyceride levels, individuals may experience acute pancreatitis, which is inflammation of the pancreas. Symptoms of pancreatitis can include severe abdominal pain, nausea, vomiting, and fever.
- Abdominal Pain: High triglyceride levels can also cause discomfort or pain in the upper abdomen, particularly after consuming a meal that is high in fat.
- Fatigue: Elevated levels of cholesterol and triglycerides can sometimes contribute to feelings of fatigue or weakness, although these symptoms are nonspecific and can have many other causes.
- Cholesterol Deposits in Blood Vessels: Over time, high blood lipids can lead to the buildup of fatty plaques in the walls of arteries, which can impair blood flow and increase the risk of cardiovascular events such as heart attacks and strokes. However, this process typically does not cause noticeable symptoms until it reaches an advanced stage.
It’s important to note that many individuals with high blood lipids may not experience any symptoms at all, making regular screening and monitoring essential for early detection and intervention. Lifestyle modifications such as adopting a heart-healthy diet, engaging in regular exercise, maintaining a healthy weight, and avoiding smoking can help lower blood lipid levels and reduce the risk of cardiovascular disease. In some cases, medication may also be prescribed to manage high blood lipids effectively.
High Cholesterol Body Symptoms:
The body serves as a canvas, painting a picture of internal health through external manifestations. High cholesterol often leaves its mark in the form of fatty deposits around the eyes, elbows, knees, and tendons—a condition known as tendon xanthomas. These visible clues serve as a stark reminder of the importance of maintaining cholesterol levels within a healthy range. High cholesterol can affect the body in various ways, and certain symptoms may manifest as a result of elevated cholesterol levels. Here are some potential physical symptoms associated with high cholesterol:
- Xanthomas: These are yellowish, fatty deposits that can develop under the skin, commonly appearing on the elbows, knees, hands, feet, or buttocks. Xanthomas may present as small bumps, nodules, or plaques and can be a visible sign of high cholesterol levels.
- Xanthelasma: Similar to xanthomas, xanthelasma are yellowish patches or plaques that form on the eyelids. These cholesterol deposits may appear as raised or flat lesions and are often indicative of elevated cholesterol levels.
- Arcus Senilis: Also known as arcus corneae or corneal arcus, this is a whitish or grayish ring that develops around the cornea of the eye. Arcus senilis results from the deposition of cholesterol in the cornea and may be more prevalent in individuals with high cholesterol levels, particularly in older adults.
- Tendon Xanthomas: These are cholesterol deposits that accumulate in tendons, causing painless but visible lumps or nodules to form. Tendon xanthomas are commonly found in the Achilles tendon (at the back of the ankle) and may be associated with conditions such as familial hypercholesterolemia.
- Corneal Arcus: A white or grayish ring around the cornea of the eye, often indicative of high cholesterol levels.
- Gallstones: High cholesterol levels can contribute to the formation of gallstones, which are solid particles that develop in the gallbladder. Gallstones may cause symptoms such as abdominal pain, nausea, vomiting, and jaundice.
- Atherosclerosis: Over time, elevated cholesterol levels can lead to the accumulation of fatty plaques in the walls of arteries, a condition known as atherosclerosis. Atherosclerosis can narrow and stiffen the arteries, impairing blood flow to vital organs and increasing the risk of cardiovascular diseases such as heart attacks and strokes.
Recognizing these physical symptoms of high cholesterol is important for early detection and intervention. Individuals experiencing any of these symptoms should consult with a healthcare professional for proper evaluation and management of their cholesterol levels. Lifestyle modifications such as adopting a heart-healthy diet, engaging in regular exercise, maintaining a healthy weight, and avoiding smoking can help lower cholesterol levels and reduce the risk of cardiovascular disease. In some cases, medication may also be prescribed to manage high cholesterol effectively.

High LDL Cholesterol Side Effects:
Low-density lipoprotein (LDL) cholesterol, commonly referred to as the “bad” cholesterol, poses significant risks when elevated. Its detrimental effects extend beyond cardiovascular health, contributing to a myriad of complications such as erectile dysfunction, peripheral artery disease, and even dementia. Keeping LDL cholesterol in check is paramount to safeguarding overall well-being. Elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, can have several adverse effects on health. Here are some potential side effects associated with high LDL cholesterol:
- Atherosclerosis: High LDL cholesterol is a major risk factor for the development of atherosclerosis, a condition characterized by the buildup of plaque in the walls of arteries. Over time, these plaques can narrow and harden the arteries, restricting blood flow to vital organs such as the heart and brain. Atherosclerosis increases the risk of cardiovascular diseases such as coronary artery disease, heart attacks, and strokes.
- Coronary Artery Disease (CAD): CAD occurs when the coronary arteries that supply blood to the heart muscle become narrowed or blocked due to atherosclerosis. High LDL cholesterol contributes to the formation of plaque in the coronary arteries, increasing the risk of angina (chest pain), heart attacks, and other complications associated with CAD.
- Peripheral Artery Disease (PAD): PAD occurs when plaque buildup restricts blood flow to the extremities, typically the legs. High LDL cholesterol can accelerate the progression of atherosclerosis in peripheral arteries, leading to symptoms such as leg pain, cramping, numbness, and weakness, especially during physical activity.
- Stroke: Atherosclerosis caused by high LDL cholesterol can also affect the arteries supplying blood to the brain, increasing the risk of ischemic stroke. An ischemic stroke occurs when a blood clot or plaque obstructs a blood vessel in the brain, depriving brain tissue of oxygen and nutrients.
- Erectile Dysfunction (ED): High LDL cholesterol can impair blood flow to the genitals, leading to erectile dysfunction in men. Reduced blood flow to the penis can interfere with the ability to achieve or maintain an erection, affecting sexual function and overall quality of life.
- Memory and Cognitive Decline: Some research suggests that high LDL cholesterol levels may be associated with an increased risk of cognitive decline and dementia in older adults. The exact mechanisms underlying this association are not fully understood but may involve impaired cerebral blood flow and the formation of plaques in brain arteries.
- Gallstones: High LDL cholesterol levels can contribute to the formation of gallstones, which are solid particles that develop in the gallbladder. Gallstones may cause symptoms such as abdominal pain, nausea, vomiting, and jaundice.
It’s important to monitor LDL cholesterol levels regularly and take steps to lower them if they are elevated. Lifestyle modifications such as adopting a heart-healthy diet, engaging in regular exercise, maintaining a healthy weight, and avoiding smoking can help reduce LDL cholesterol levels and lower the risk of associated complications. In some cases, medication may also be prescribed to manage high LDL cholesterol effectively.

Overweight Cholesterol:
Excess weight not only takes a toll on physical appearance but also wreaks havoc on internal health, including cholesterol levels. Obesity is often associated with unfavorable lipid profiles, characterized by elevated LDL cholesterol and triglycerides, coupled with reduced levels of beneficial high-density lipoprotein (HDL) cholesterol. Shedding excess pounds through a balanced diet and regular exercise is key to reversing this dangerous trend. Being overweight or obese can significantly impact cholesterol levels and overall cardiovascular health. Here’s how excess weight can affect cholesterol:
- Increased LDL Cholesterol: Excess body weight, especially abdominal obesity, is associated with elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. High LDL cholesterol increases the risk of atherosclerosis and cardiovascular diseases such as heart attacks and strokes.
- Reduced HDL Cholesterol: Being overweight or obese can lower levels of high-density lipoprotein (HDL) cholesterol, known as “good” cholesterol. HDL cholesterol helps remove LDL cholesterol from the bloodstream, reducing the risk of plaque buildup in the arteries. Low HDL cholesterol levels are a significant risk factor for heart disease.
- Increased Triglycerides: Excess weight is often associated with elevated levels of triglycerides, a type of fat found in the blood. High triglyceride levels, combined with high LDL cholesterol and low HDL cholesterol, contribute to the development of atherosclerosis and increase the risk of cardiovascular events.
- Insulin Resistance: Obesity is closely linked to insulin resistance, a condition in which cells become less responsive to the effects of insulin. Insulin resistance can lead to dyslipidemia, characterized by elevated levels of triglycerides and LDL cholesterol, as well as reduced levels of HDL cholesterol. Dyslipidemia further increases the risk of cardiovascular disease.
- Inflammation: Adipose (fat) tissue produces inflammatory substances that can promote atherosclerosis and impair cholesterol metabolism. Chronic inflammation associated with obesity contributes to the progression of cardiovascular disease and other metabolic disorders.
- Fatty Liver Disease: Obesity increases the risk of non-alcoholic fatty liver disease (NAFLD), a condition characterized by the accumulation of fat in the liver. NAFLD is associated with dyslipidemia, insulin resistance, and elevated levels of LDL cholesterol and triglycerides, increasing the risk of cardiovascular complications.
- Reduced Response to Cholesterol-Lowering Treatment: Individuals who are overweight or obese may have a reduced response to cholesterol-lowering medications such as statins. Lifestyle modifications, including weight loss through diet and exercise, are often recommended as first-line therapy to improve cholesterol levels in these individuals.
Addressing overweight and obesity is essential for managing cholesterol levels and reducing the risk of cardiovascular disease. Adopting a healthy lifestyle that includes a balanced diet, regular physical activity, stress management, and adequate sleep can help achieve and maintain a healthy weight and improve overall cardiovascular health. Additionally, seeking guidance from healthcare professionals for personalized recommendations and support is crucial in managing weight and cholesterol effectively.
Cardiovascular Disease and Cholesterol:
Cardiovascular disease lurks in the shadows, claiming lives silently and swiftly. Cholesterol, particularly LDL cholesterol, plays a central role in its development, contributing to the formation of arterial plaques that narrow blood vessels and increase the risk of catastrophic events. Prioritizing heart health through lifestyle modifications and cholesterol management is paramount in combating this prevalent threat.
In partnership with Dr. Cynthia, a renowned expert in cardiovascular health, we emphasize the importance of proactive measures in tackling cholesterol-related issues. Through education, awareness, and actionable steps, individuals can take charge of their health destiny and pave the way for a heart-healthy future. Cholesterol plays a pivotal role in the development of cardiovascular disease (CVD), which encompasses a range of conditions affecting the heart and blood vessels. Here’s how cholesterol contributes to CVD:
- Atherosclerosis: High levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, contribute to the formation of plaque in the walls of arteries. This process, known as atherosclerosis, narrows and stiffens the arteries, reducing blood flow to vital organs such as the heart and brain. Atherosclerosis is a key underlying cause of various cardiovascular conditions, including coronary artery disease (CAD), peripheral artery disease (PAD), and cerebrovascular disease.
- Coronary Artery Disease (CAD): CAD occurs when plaque buildup narrows the coronary arteries that supply oxygen-rich blood to the heart muscle. Reduced blood flow to the heart can lead to chest pain (angina), shortness of breath, and, in severe cases, heart attacks (myocardial infarctions). High LDL cholesterol levels are a major risk factor for CAD, while low levels of high-density lipoprotein (HDL) cholesterol, or “good” cholesterol, further exacerbate the risk.
- Heart Attacks and Strokes: Rupture or erosion of atherosclerotic plaques can trigger the formation of blood clots, which can obstruct blood flow to the heart (causing a heart attack) or brain (leading to a stroke). High LDL cholesterol levels increase the likelihood of plaque instability and clot formation, while low HDL cholesterol levels impair the body’s ability to remove cholesterol from arterial walls, further increasing the risk of cardiovascular events.
- Peripheral Artery Disease (PAD): Atherosclerosis can also affect arteries outside the heart, leading to PAD. In PAD, narrowed arteries reduce blood flow to the extremities, typically the legs, causing symptoms such as leg pain, cramping, numbness, and weakness, especially during physical activity. High cholesterol levels contribute to the progression of PAD and increase the risk of complications such as non-healing wounds and limb ischemia.
- Ischemic Heart Failure: Chronic narrowing of coronary arteries due to atherosclerosis can impair blood flow to the heart muscle, leading to ischemic heart failure. In this condition, the heart becomes progressively weakened and unable to pump blood effectively, resulting in symptoms such as fatigue, shortness of breath, and fluid retention. High cholesterol levels contribute to the development and progression of ischemic heart failure by exacerbating coronary artery disease.
- Management and Prevention: Lowering cholesterol levels, particularly LDL cholesterol, is a cornerstone of preventing and managing CVD. Lifestyle modifications, including adopting a heart-healthy diet low in saturated and trans fats, engaging in regular physical activity, maintaining a healthy weight, quitting smoking, and managing stress, are crucial for reducing cholesterol levels and mitigating the risk of cardiovascular events. Additionally, medications such as statins may be prescribed to further lower cholesterol levels and prevent CVD in high-risk individuals.
Cholesterol plays a central role in the pathogenesis of cardiovascular disease, including atherosclerosis, coronary artery disease, peripheral artery disease, heart attacks, strokes, and heart failure. By addressing high cholesterol levels through lifestyle modifications and appropriate medical management, individuals can significantly reduce their risk of developing cardiovascular disease and improve their overall heart health. Regular monitoring of cholesterol levels and adherence to preventive measures are essential for maintaining cardiovascular health and preventing potentially life-threatening complications.