Coronary artery disease (CAD) is a leading cause of mortality worldwide, and while it’s often associated with men, it’s crucial to recognize that females are equally susceptible. Understanding the symptoms of CAD in females is paramount for early detection and timely intervention. Recognizing the symptoms of coronary artery disease in females is paramount for early detection and intervention. By understanding the unique presentation of CAD in women and addressing gender disparities in healthcare, we can improve outcomes and save lives.
Prevalence of CAD in Females
Coronary artery disease (CAD) affects millions of women worldwide, making it a significant health concern. Despite historically being viewed as primarily a male issue, CAD is increasingly recognized as a serious threat to women’s health. As women age, especially after menopause, their risk of developing CAD rises, often due to hormonal changes and other factors. It’s crucial to understand the prevalence of CAD in females to address this health issue effectively.
Common Symptoms of CAD in Females
Recognizing the symptoms of coronary artery disease (CAD) in females is essential for early detection and treatment. While some symptoms may overlap with those experienced by males, females may also present with unique signs. Here are some common symptoms of CAD in females to watch out for:
- Chest Pain and Discomfort: Chest pain or discomfort, often described as pressure, tightness, squeezing, or burning sensation, is a hallmark symptom of CAD in both males and females. However, women may experience atypical chest pain that differs from the classic “crushing” sensation often associated with heart attacks.
- Shortness of Breath: Unexplained shortness of breath, particularly during physical exertion or even at rest, can be a sign of reduced blood flow to the heart muscles. This symptom may occur without any apparent cause and may worsen over time.
- Fatigue and Weakness: Persistent fatigue and weakness, even with minimal physical activity, may indicate reduced cardiac function due to CAD. Women may feel unusually tired despite getting enough rest, which can affect their daily activities and quality of life.
- Nausea and Indigestion: CAD can sometimes manifest as gastrointestinal symptoms such as nausea, vomiting, or indigestion, especially in females. These symptoms may occur without any accompanying chest pain and are often overlooked or misinterpreted.
- Jaw, Neck, or Back Pain: Women with CAD may experience pain or discomfort in areas other than the chest, such as the jaw, neck, shoulders, arms, or upper back. This radiating pain may be mistaken for muscle strain or tension but can be a sign of underlying heart issues.
It’s important to note that while these symptoms are common in females with CAD, not all women will experience them. Some individuals may have no symptoms at all, especially in the early stages of the disease. Therefore, any unusual or concerning symptoms should be promptly evaluated by a healthcare professional to rule out or confirm CAD and initiate appropriate treatment. Early detection and intervention can significantly improve outcomes and reduce the risk of complications associated with CAD.
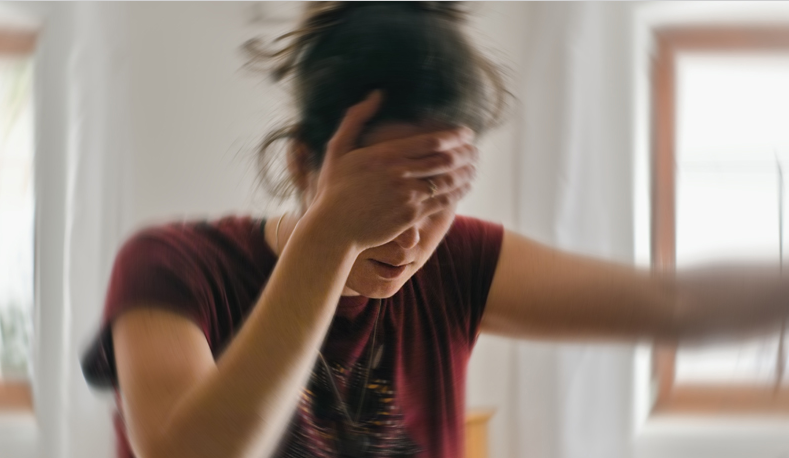
Atypical Symptoms in Females
Women with CAD may not always experience typical chest pain. Instead, they might present with atypical symptoms like unexplained fatigue, anxiety, or sleep disturbances. These subtle signs often lead to misdiagnosis or delayed treatment. The common symptoms associated with coronary artery disease (CAD), females may also experience atypical or less typical symptoms. These atypical symptoms can be subtle and may not always raise immediate concern, leading to underdiagnosis or delayed treatment. It’s essential to recognize these signs to ensure timely intervention and better outcomes for women with CAD. Here are some atypical symptoms commonly observed in females:
- Absence of Chest Pain: Unlike men, women with CAD may not always experience chest pain or discomfort. Instead, they may present with other symptoms such as shortness of breath, fatigue, or nausea without any accompanying chest discomfort. This lack of chest pain can make it challenging to recognize CAD in females, leading to delayed diagnosis and treatment.
- Unexplained Fatigue: Persistent and unexplained fatigue is a common atypical symptom of CAD in females. Women may feel excessively tired, even after getting enough rest, and may find it difficult to perform routine activities. This fatigue may be disproportionate to the level of exertion and may not improve with rest.
- Anxiety or Sleep Disturbances: Some females with CAD may experience symptoms such as anxiety, restlessness, or sleep disturbances. These psychological symptoms may be related to the underlying cardiac condition and can significantly impact a woman’s overall well-being and quality of life. However, they are often overlooked or attributed to other causes, delaying the diagnosis of CAD.
Recognizing these atypical symptoms is crucial for healthcare providers and women themselves to identify CAD early and initiate appropriate management. Women should pay attention to any unusual or persistent symptoms and seek medical attention if they have concerns about their heart health. By raising awareness about these atypical symptoms, we can improve the timely diagnosis and treatment of CAD in females, ultimately reducing the burden of this disease on women’s health.
Challenges in Diagnosis
Diagnosing coronary artery disease (CAD) in females presents several challenges due to various factors, including symptom variation, lack of awareness, and underrecognition by healthcare providers. These challenges contribute to delayed diagnosis and treatment, potentially leading to adverse outcomes for women with CAD. Understanding and addressing these diagnostic challenges are crucial for improving the management of CAD in females. Here are some key challenges in diagnosing CAD in women:
- Symptom Variation: Females with CAD often present with atypical or less typical symptoms compared to men, such as absence of chest pain, unexplained fatigue, or gastrointestinal symptoms. This variation in symptom presentation can lead to underrecognition by both patients and healthcare providers, delaying the diagnosis of CAD.
- Lack of Awareness: There is a general lack of awareness about the prevalence and risk of CAD in females, both among the public and healthcare professionals. As a result, women may not recognize the symptoms of CAD or may attribute them to other causes, leading to delays in seeking medical attention.
- Misinterpretation of Symptoms: Healthcare providers may misinterpret or dismiss the symptoms reported by female patients, especially if they do not fit the traditional presentation of CAD. This can result in missed opportunities for early diagnosis and intervention, putting women at risk of complications.
- Delayed Diagnosis and Treatment: Due to the challenges mentioned above, Coronary Artery Disease is often diagnosed later in females compared to males. Delayed diagnosis can lead to progression of the disease, increased risk of heart attacks or strokes, and poorer outcomes for women with CAD.
Addressing these challenges requires efforts to increase awareness about Coronary Artery Disease in females among both the general public and healthcare professionals. Education and training programs aimed at recognizing atypical symptoms and risk factors specific to women can help improve early detection and management of CAD. Additionally, promoting gender-sensitive approaches to healthcare delivery and ensuring equitable access to diagnostic tests and treatments are essential steps in overcoming the challenges in diagnosing Coronary Artery Disease in females. By addressing these barriers, we can enhance the quality of care and outcomes for women with CAD, ultimately reducing the burden of this disease on female health.

Importance of Early Detection
Early detection of CAD in females is critical for preventing adverse outcomes. Timely intervention can mitigate the risk of heart attacks, strokes, and other complications, ultimately improving quality of life.
Early detection of coronary artery disease (CAD) in women is paramount to initiate timely intervention and prevent adverse outcomes. Despite the challenges in diagnosing CAD in women, early identification of the disease can significantly improve prognosis and quality of life. Here are several reasons why early detection is important:
- Preventing complications: Early detection allows treatment and lifestyle changes to begin immediately, reducing the risk of complications such as heart attack, stroke, and heart failure. By treating CAD in the early stages, women can avoid disease progression and its associated complications.
- Improves prognosis: Timely intervention can improve the prognosis of CAD in women by slowing the progression of the disease and preventing further damage to the heart. Early detection enables healthcare providers to implement appropriate treatment strategies tailored to the individual needs of the patient, leading to better outcomes.
- Enhanced quality of life: CAD can significantly impact a woman’s quality of life, affecting her ability to perform daily activities and engage in social and recreational activities. Early detection and management of CAD can reduce symptoms, improve functional ability, and increase overall well-being, allowing women to live full lives.
- Reducing health care costs: Early detection and treatment of CAD can help reduce health care costs associated with managing advanced stages of the disease and its complications. By investing in preventive measures and early intervention, healthcare systems can achieve cost savings and allocate resources more efficiently.
- Empowering Patients: Early detection empowers women to take control of their heart health and make informed decisions about their lifestyle and treatment options. By raising awareness about the importance of recognizing CAD symptoms and seeking timely medical help, women can advocate for their health and well-being.
Overall, early detection of CAD in women may have significant benefits, including preventing complications, improving prognosis, increasing quality of life, reducing health care costs, and empowering patients. Healthcare providers, policy makers, and community stakeholders play an important role in promoting awareness, facilitating early diagnosis, and ensuring access to comprehensive care for women with CAD. By prioritizing early detection efforts, we can make progress in reducing the burden of CAD on women’s health and improving outcomes for women at risk for or living with the disease.

Risk Factors for CAD in Females
Coronary artery disease (CAD) in females can result from a combination of genetic, lifestyle, and environmental factors. Recognizing these risk factors is essential for early prevention and intervention. While some risk factors for CAD are common to both genders, others may affect women differently or have a more significant impact on their cardiovascular health. Here are some key risk factors for CAD in females:
- Age: As women age, their risk of developing CAD increases, particularly after menopause. Hormonal changes associated with menopause, such as a decrease in estrogen levels, can contribute to changes in lipid profile and blood pressure, increasing the risk of CAD.
- Family History: A family history of CAD or cardiovascular events, especially in first-degree relatives (parents or siblings), can significantly increase a woman’s risk of developing the disease. Genetic predisposition plays a crucial role in CAD risk and should be considered in risk assessment and preventive strategies.
- Lifestyle Factors: Unhealthy lifestyle habits, such as smoking, poor diet, physical inactivity, and excessive alcohol consumption, can significantly elevate the risk of CAD in females. Smoking, in particular, is a potent risk factor for CAD and has been associated with a higher risk of heart disease in women compared to men.
- Obesity and Metabolic Syndrome: Obesity, especially abdominal or central obesity, is a significant risk factor for CAD in females. Excess body weight, particularly visceral fat, is associated with insulin resistance, dyslipidemia, hypertension, and inflammation, collectively known as metabolic syndrome, which further increases CAD risk.
- Diabetes: Women with diabetes are at a higher risk of developing CAD compared to those without diabetes. Diabetes increases the risk of atherosclerosis (hardening and narrowing of the arteries), leading to reduced blood flow to the heart and an increased risk of heart attacks and other cardiovascular events.
- Hypertension: High blood pressure (hypertension) is a major risk factor for CAD in females. Elevated blood pressure puts added strain on the heart and blood vessels, increasing the risk of atherosclerosis and cardiovascular complications over time.
- High Cholesterol Levels: Elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, and reduced levels of high-density lipoprotein (HDL) cholesterol, or “good” cholesterol, are associated with an increased risk of CAD in females. Dyslipidemia contributes to the development of atherosclerosis and coronary artery plaque buildup.
- Other Health Conditions: Certain health conditions, such as chronic kidney disease, autoimmune disorders (e.g., rheumatoid arthritis, systemic lupus erythematosus), and mental health disorders (e.g., depression, anxiety), may increase the risk of CAD in females. These conditions often coexist with traditional CAD risk factors and can exacerbate cardiovascular risk.
Recognizing these risk factors and addressing modifiable factors through lifestyle modifications, preventive measures, and medical management are essential for reducing the risk of CAD in females. Healthcare providers play a crucial role in conducting risk assessments, providing personalized recommendations, and promoting cardiovascular health education to empower women to take proactive steps toward heart disease prevention.

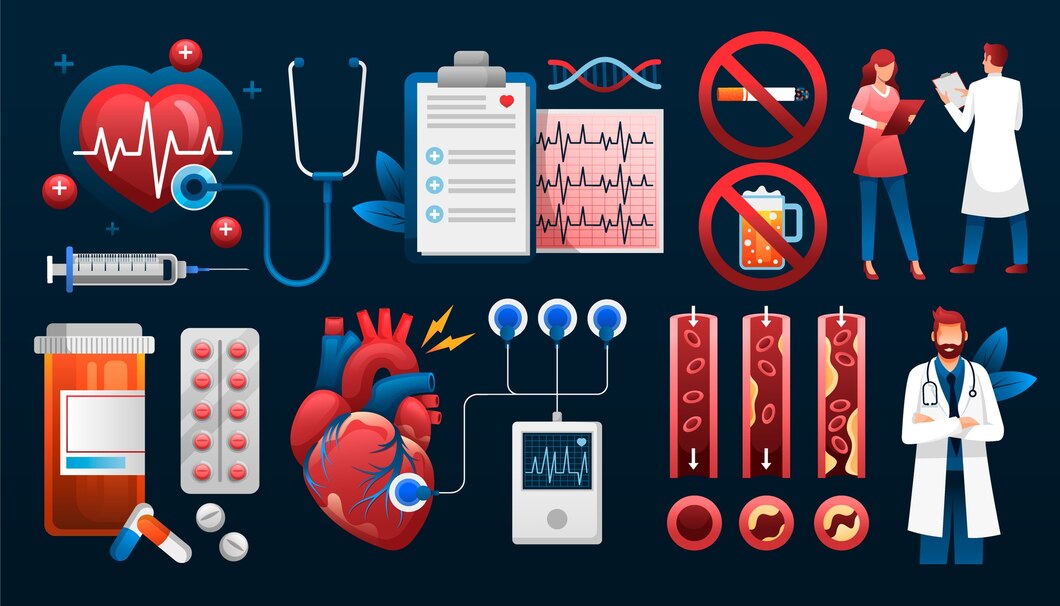
Diagnostic Tests for CAD
Diagnosing coronary artery disease (CAD) in females requires a comprehensive approach that combines clinical evaluation, medical history assessment, and diagnostic testing. Various diagnostic tests are available to evaluate cardiac function, assess the extent of coronary artery blockages, and confirm the presence of CAD. Here are some common diagnostic tests used in the evaluation of CAD in females:
- Electrocardiogram (ECG or EKG): An electrocardiogram records the electrical activity of the heart and can detect abnormalities such as irregular heart rhythms, ischemic changes, and signs of previous heart attacks. While an ECG is a valuable screening tool, it may not always detect CAD, especially in women with atypical symptoms.
- Echocardiogram (Echo): An echocardiogram uses sound waves to create images of the heart’s structure and function. It can assess cardiac chambers, valves, and overall heart function, helping identify abnormalities such as reduced heart muscle function (e.g., left ventricular dysfunction) or structural heart defects that may be associated with CAD.
- Stress Tests: Stress tests evaluate how well the heart performs under physical stress and can help detect CAD-related abnormalities. Exercise stress tests involve walking on a treadmill or using a stationary bike while monitoring heart rate, blood pressure, and ECG changes. Nuclear stress tests or stress echocardiograms may be performed in conjunction with exercise or pharmacological stress agents to assess blood flow to the heart during stress.
- Cardiac Catheterization (Coronary Angiography): Cardiac catheterization involves inserting a catheter into the coronary arteries and injecting contrast dye to visualize the blood flow and detect blockages or narrowing of the arteries. Coronary angiography is considered the gold standard for diagnosing CAD and is often performed in conjunction with other procedures, such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
- Computed Tomography Angiography (CTA): Computed tomography angiography uses CT imaging to create detailed images of the coronary arteries and detect blockages or plaques. CTA is a non-invasive alternative to traditional cardiac catheterization and may be used for CAD diagnosis in select cases, particularly in individuals with low to intermediate risk of CAD.
- Coronary Calcium Scoring: Coronary calcium scoring measures the amount of calcium deposits in the coronary arteries, which can indicate the presence of atherosclerosis and CAD. This non-invasive imaging test, often performed using computed tomography (CT), provides valuable information about the extent of coronary artery calcification and helps assess CAD risk.
- Fractional Flow Reserve (FFR): Fractional flow reserve is an invasive procedure used during cardiac catheterization to assess the functional significance of coronary artery blockages. FFR measures the pressure difference across a narrowing in the coronary artery to determine if it is causing significant blood flow restriction and requires intervention.
These diagnostic tests play a crucial role in evaluating CAD in females, aiding in diagnosis, risk stratification, and treatment decision-making. Healthcare providers may recommend specific tests based on individual patient characteristics, symptoms, risk factors, and clinical presentation. Early detection and accurate diagnosis of CAD in females enable timely intervention and improve outcomes, reducing the risk of complications and enhancing overall cardiovascular health.

Treatment Options
The management of coronary artery disease (CAD) in females involves a multifaceted approach aimed at reducing symptoms, preventing disease progression, and minimizing the risk of cardiovascular events. Treatment strategies for CAD in females may include lifestyle modifications, medications, invasive procedures, and surgical interventions tailored to individual patient needs and preferences. Here are some common treatment options for CAD in females:
- Lifestyle Modifications:
- Healthy Diet: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help reduce cholesterol levels, blood pressure, and inflammation, lowering the risk of CAD progression.
- Regular Exercise: Engaging in regular physical activity, such as brisk walking, cycling, or swimming, promotes cardiovascular health, improves circulation, and helps manage weight, blood sugar, and stress levels.
- Smoking Cessation: Quitting smoking and avoiding exposure to secondhand smoke are crucial for reducing the risk of CAD and improving overall cardiovascular health.
- Medications:
- Cholesterol-Lowering Medications: Statins are commonly prescribed to lower LDL cholesterol levels and reduce the risk of atherosclerosis progression and cardiovascular events. Other medications, such as ezetimibe or PCSK9 inhibitors, may be used in combination with statins for additional lipid-lowering effects.
- Antiplatelet Agents: Aspirin and other antiplatelet medications may be prescribed to reduce the risk of blood clot formation and prevent heart attacks and strokes in individuals with CAD.
- Blood Pressure Medications: Antihypertensive medications, such as ACE inhibitors, beta-blockers, calcium channel blockers, or diuretics, help control high blood pressure and reduce the risk of CAD-related complications.
- Antianginal Medications: Nitroglycerin and other antianginal medications may be prescribed to relieve chest pain (angina) and improve blood flow to the heart muscle.
- Invasive Procedures:
- Percutaneous Coronary Intervention (PCI): PCI, also known as angioplasty, involves inserting a catheter with a balloon into the blocked coronary artery to widen it and improve blood flow. In some cases, a stent may be placed to keep the artery open and prevent re-narrowing.
- Coronary Artery Bypass Grafting (CABG): CABG is a surgical procedure that involves bypassing blocked coronary arteries using blood vessels harvested from other parts of the body, such as the chest or leg. CABG is typically reserved for individuals with complex CAD or those who do not respond to medical therapy or PCI.
- Cardiac Rehabilitation:
- Exercise Training: Cardiac rehabilitation programs offer supervised exercise training tailored to individual fitness levels and cardiac conditions, helping improve cardiovascular fitness, reduce symptoms, and enhance overall well-being.
- Education and Counseling: Cardiac rehabilitation programs provide education and counseling on heart-healthy lifestyle habits, medication management, stress reduction, and emotional support to empower individuals to manage their CAD effectively.
- Secondary Prevention Measures:
- Routine Medical Follow-up: Regular medical follow-up appointments with healthcare providers are essential for monitoring CAD progression, adjusting treatment plans, and addressing any emerging issues or concerns.
- Risk Factor Modification: Continuously optimizing risk factors such as blood pressure, cholesterol levels, blood sugar, and weight through lifestyle modifications and medication management helps reduce the risk of recurrent cardiovascular events.
- Psychosocial Support: Addressing psychosocial factors such as stress, anxiety, depression, and social isolation through counseling, support groups, or mental health services can improve overall well-being and quality of life in individuals with CAD.
By implementing a comprehensive treatment approach that addresses modifiable risk factors, optimizes medical therapy, and utilizes appropriate interventions, healthcare providers can effectively manage CAD in females and improve long-term outcomes. Patient education, empowerment, and engagement are integral components of CAD management, enabling women to take an active role in their cardiovascular health and reduce the burden of this disease.
Preventive Measures
Preventing coronary artery disease (CAD) in females involves adopting a proactive approach to cardiovascular health and implementing preventive measures aimed at reducing risk factors and promoting overall well-being. By focusing on lifestyle modifications, regular screening, and early intervention, women can significantly lower their risk of developing CAD and improve their heart health. Here are some preventive measures to consider:
- Healthy Diet:
- Emphasize a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limit intake of saturated and trans fats, cholesterol, sodium, and refined sugars.
- Choose heart-healthy cooking methods such as baking, grilling, steaming, or roasting instead of frying.
- Monitor portion sizes and practice mindful eating to avoid overeating and maintain a healthy weight.
- Regular Exercise:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week.
- Incorporate activities that promote cardiovascular fitness, such as walking, jogging, cycling, swimming, or dancing.
- Include strength training exercises at least two days per week to improve muscle strength and endurance.
- Stay active throughout the day by taking short walks, using stairs instead of elevators, or engaging in household chores or gardening.
- Smoking Cessation:
- Quit smoking and avoid exposure to secondhand smoke, which increases the risk of CAD and other cardiovascular diseases.
- Seek support from healthcare providers, smoking cessation programs, or support groups to develop a quit plan and address nicotine addiction.
- Maintain a Healthy Weight:
- Achieve and maintain a healthy body weight by balancing caloric intake with physical activity.
- Aim for a body mass index (BMI) within the normal range (18.5-24.9 kg/m²) and waist circumference below 35 inches for women.
- Manage Stress:
- Practice stress-reduction techniques such as deep breathing, meditation, yoga, tai chi, or progressive muscle relaxation.
- Prioritize self-care activities, hobbies, and leisure pursuits to promote relaxation and mental well-being.
- Seek professional help or counseling if experiencing chronic stress, anxiety, or depression.
- Regular Health Screenings:
- Schedule regular check-ups with healthcare providers for preventive screenings and assessments of blood pressure, cholesterol levels, blood sugar, and weight.
- Follow recommended guidelines for age-appropriate screenings such as mammograms, Pap smears, and bone density tests.
- Medication Adherence:
- Take prescribed medications as directed by healthcare providers to manage underlying health conditions and reduce cardiovascular risk.
- Discuss any concerns or side effects with healthcare providers and adhere to medication regimens to optimize treatment outcomes.
- Limit Alcohol Consumption:
- Drink alcohol in moderation, if at all, and limit intake to no more than one drink per day for women.
- Avoid binge drinking and excessive alcohol consumption, which can increase the risk of CAD, high blood pressure, and other health problems.
By incorporating these preventive measures into daily life and maintaining a heart-healthy lifestyle, women can reduce their risk of developing CAD and promote overall cardiovascular health. It’s essential to prioritize self-care, regular health screenings, and adherence to medical recommendations to achieve long-term wellness and vitality.
Support and Resources
Access to patient education, support groups, and online resources empowers women to manage CAD effectively and navigate their healthcare journey.
Addressing Gender Disparities
Efforts to address gender disparities in CAD diagnosis and treatment involve advocacy, research, and healthcare provider training to improve awareness and outcomes among females.
FAQs
- What are the early signs of CAD in females? Early signs may include chest discomfort, shortness of breath, fatigue, nausea, and jaw or back pain.
- Can CAD occur without chest pain in females? Yes, females may experience atypical symptoms like fatigue, shortness of breath, or indigestion without chest pain.
- How can lifestyle changes help prevent CAD in females? Lifestyle changes such as maintaining a healthy diet, regular exercise, quitting smoking, and managing stress can significantly reduce CAD risk in females.
- Are women more likely to die from CAD than men? CAD mortality rates in women have been historically lower than in men, but this gap is narrowing due to increased awareness and improved treatments.
- What should I do if I suspect CAD symptoms in myself or a loved one? If you or someone you know experiences symptoms suggestive of CAD, seek medical attention promptly. Early diagnosis and treatment are vital for better outcomes.